- Student/Faculty Portal
- Learning Hub (Brightspace)
- Continuous Professional Development
- Admissions and Application Process
- Prerequisites and Requirements
- Financial Support
- Curriculum Overview
- Initiative for Maximizing Student Development (IMSD)
- Career Development Internships
- Tracks Overview
- Biochemistry and Molecular Biology
- Biomedical Engineering and Physiology
- Clinical and Translational Science
- Molecular Pharmacology and Experimental Therapeutics
- Neuroscience

Regenerative Sciences
- Virology and Gene Therapy
- Find a Mentor
- Student Life Overview
- Student Spotlights
- Student Organizations
- Graduate Student Workspaces
- Events and Programs
- Alumni Perspectives
- Student Research
Regenerative Sciences Track
faculty spanning multidisciplinary departments
education in discovery, clinical translation, and application of regenerative solutions
Guaranteed 5-year internal fellowship
includes full tuition, stipend and benefits
Seeking to spur development of innovative medical breakthroughs, Mayo Clinic Graduate School of Biomedical Sciences, in partnership with the Center for Regenerative Biotherapeutics , started one of the nation's first doctoral research training programs in regenerative sciences.
Regenerative medicine is transforming clinical practice with the development of new therapies, treatments and surgeries for patients with chronic conditions, debilitating injuries and degenerative diseases. Advances in developmental and cell biology, immunology, and other fields unlock new opportunities for innovative breakthroughs for the next generation of regenerative diagnostic and therapeutic medical solutions.
The Regenerative Sciences (REGS) Ph.D. track at Mayo Clinic is a transdisciplinary Ph.D. Program designed to prepare the next generation of scientists to accelerate the discovery, translation, and application of cutting-edge regenerative diagnostics and therapeutics. The REGS Ph.D. track builds on the existing Mayo Clinic Regenerative Sciences Training Program (RSTP) to now offer in-depth curriculum and advanced training opportunities.
The Regenerative Sciences Track places a significant emphasis on laboratory-based research training. Laboratory research is complemented with both core and track-specific courses, as well as advanced courses on current topics in regenerative science and medicine.
The regenerative sciences curriculum encompasses the full spectrum of regenerative science topics, including molecular and cell biology, stem cell biology, developmental biology, tissue engineering, biomaterials and nanomedicine, genome editing and gene therapies, regulatory and translational science, product development, biomanufacturing, entrepreneurship and more.
Students in Regenerative Sciences join a close-knit community of learners, are provided unique hands-on- experiences and collaborate with some of the brightest minds in the field.
See the full Regenerative Sciences Track curriculum (PDF)
Graduates of the Regenerative Sciences Ph.D. track will be integral to forming the multidisciplinary workforce needed to drive the future of health care at Mayo Clinic and across the world.
Learn more: What is Regenerative Medicine - Mayo Clinic Radio
Focus areas
- Molecular and epigenetic mechanisms of stem and progenitor cell proliferation and differentiation, as well as tissue degeneration and regeneration
- Immune responses to viral insult and tissue healing
- Gene editing for cell therapy applications and to alter disease progression
- Extracellular vesicles in disease progression and for tissue regeneration
- Tissue engineering and bioengineering of novel therapies, including 3-D printing, electrospinning, and advanced biomanufacturing
/0x0:512x512/prod01/channel_2/media/mccms/content-assets/academics/biomedical-research-training/phd-program/curriculumx2ftracks/ShanGao_512X512.jpg)
Mayo Clinic is an incredible place for doctoral training in regenerative science. The interdisciplinary strategy here allows research and courses to be tailored according to each student’s interests and ability. Moreover, Mayo Clinic provides a wealth resource to develop collaborations within the institution, which will offer students more ways to communicate and promote students to achieve their personal goals.
Shan Gao Ph.D. student, Regenerative Sciences Track
/0x0:512x512/prod01/channel_2/media/mccms/content-assets/academics/biomedical-research-training/phd-program/Armin-Garmany-512X512.jpg)
Mayo Clinic provides unparalleled access to world-renowned clinicians and researchers all focused on clinically relevant research. Mayo Clinic’s Center for Regenerative Medicine permeates throughout the institution. Thus, the REGS program gives students the necessary experience and knowledge to drive future research in restoring form and function in any field of medicine.
Armin Garmany M.D.-Ph.D. student, Regenerative Sciences Track
/0x0:512x512/prod01/channel_2/media/mccms/content-assets/academics/biomedical-research-training/phd-program/curriculumx2ftracks/SamuelBuchl_512X512.jpg)
The study of Regenerative Sciences (REGS) at Mayo Clinic is unparalleled. Students are funded to study cutting-edge biomedical science in their domain of interest with plentiful opportunities to translate benchside discoveries to the patient bedside and beyond. I chose Mayo Clinic's REGS program to join its community of researchers, practitioners, and entrepreneurs who everyday advance the science and practice of regenerative medicine and bring new regenerative solutions to the world.
Samuel Buchl Ph.D. student, Regenerative Sciences Track
/0x0:512x512/prod01/channel_2/media/mccms/content-assets/academics/biomedical-research-training/phd-program/curriculumx2ftracks/DelaneyLiskey_512X512.jpg)
The Regenerative Sciences Ph.D. track at Mayo Clinic thoroughly equips students to be leaders in biomedical research through an unmatched curriculum of multidisciplinary science and world-class research training. REGS is a collaborative and supportive program in a promising field of medicine that provides the foundational skills to pipeline research to patient care.
Delaney Liskey Ph.D. student, Regenerative Sciences Track
Thesis topics
Current students thesis topics.
- "Targeted Regenerative Therapies for Heart Failure Susceptibility," Armin Garmany (Mentor: Andre Terzic, M.D., Ph.D.)
- "Novel Look Into the Crude Stromal Vascular Fraction (SVF) from Human Adipose-Derived Tissue and Its Role in Regulating the Self-Renewing Capacity of Brain Tumor-Initiating Cells," Rawan Alkharboosh (Mentor: Alfredo Quinones-Hinojosa, M.D.)
- "Tissue Quality in Existing and Emerging Treatments for Osteoarthritis," Katherine Arnold (Mentor: Jennifer Westendorf, Ph.D.)
- "Harnessing the Mesenchymal Stem Cell Secretome to Target Alpha-Synuclein-Associated Dysfunction in Parkinson's Disease," Jeremy Burgess (Mentor: Pamela McLean, Ph.D.)
- "Retinal Neuroprotection Properties of an ATP-Sensitive Potassium Channel Opener," Catherine Knier (Mentor: Michael Fautsch, Ph.D.)
- "Towards a Subcutaneous Combination Biodevice for the Treatment of Type 1 Diabetes," Ethan Law (Mentor: Quinn Peterson, Ph.D.)
- "Modulation of CART Cell Activation to Enhance Antitumor Response via CRISPR-mediated Gene Editing and Combined Immunotherapy," Claudia Manriquez Roman (Mentor: Saad Kenderian, M.B., Ch.B.)
- "Systems Biology for Engineering Regenerative Immunotherapies in Precision Neuro-oncology," Dileep Monie (Mentors: Hu Li, Ph.D. and Richard Vile, Ph.D.
- "APOE2 Effects on Central and Peripheral Vasculature," Francis Shue (Mentor: Guojun Bu, Ph.D.)
- "Engineering of Antiviral Extracellular Vesicles," Amanda Terlap (Mentor: Atta Behfar, M.D., Ph.D.)
- "Glycome of Breast Cancer-Derived Extracellular Vesicles in Metastasis," Sierra Walker (Mentor: Joy Wolfram, Ph.D.)
- "Bidirectional Interactions Between Stem Cell Populations of the Subventricular Zone and Glioblastoma," Emily Norton (Mentor: Hugo Guerrero Cazares, M.D., Ph.D.)
- "Measles Virus Vector for Gene Editing and Reprogramming of Human Fibroblasts," Ramya Rallabandi (Mentor: Patricia Devaux, Ph.D.)
- "Precise Genetic Engineering of Human Primary Cells for Cell Therapy-Based Applications," (Mentor: Stephen Ekker, Ph.D.)
Recent graduates thesis topics
- "Epigenetic Control of the Architectural and Trophic Functions of Mesenchymal Stem Cells in Musculoskeletal Tissue Regeneration Therapies," (Mentor: Andre van Wijnen, Ph.D.)
- "Metabolic Regulation of Muscle Stem Cells," (Mentor: Jason Doles, Ph.D.)
- "Purified Exosome Product Enhances Neovascularization in Peripheral Arterial Disease," (Mentors: Atta Behfar, M.D., Ph.D. and Andre Terzic, M.D., Ph.D.)
- "Antigen Presentation by CNS-Resident Microglia and Macrophages is Required for Antigen-Specific CD8 T Cell Responses in the Brain Following Viral Challenge," (Mentor: Aaron Johnson, Ph.D.)
Meet the director

Training opportunities extend from fundamental science principles through laboratory skills and hands-on experiences. Students will also have the opportunity to develop an understanding of national and international regulatory agencies, and business requirements and procedures needed to implement the discovery, translation, application pipeline for new regenerative technologies.
We are excited to provide a program of training that will serve as an incubator to develop the next generation of leaders in regenerative science and medicine.
Hugo Guerrero Cazares, MD, PhD Regenerative Sciences Program Director Associate Professor of Neurosurgery Phone: 904-953-0118 Email: [email protected] See research interests
Browse a list of Regenerative Sciences Track faculty members
Updates on COVID-19 for Grad Students and Postdocs
Graduate program in stem cell biology & regenerative medicine, stanford is a world leader in stem cell research and regenerative medicine. central discoveries in stem cell biology – tissue stem cells and their use for regenerative therapies, transdifferentiation into mature cell-types, isolation of cancerous stem cells, and stem cell signaling pathways – were made by stanford faculty and students. our mission is to train the next generation of stem cell scientists..
About the SCBRM Graduate Program
Unique Opportunities for Medical Students

Stem Cell PhD Program

Faculty and Their Research Interests

Application Process
Curriculum and Handbooks
Learn about the many ways to support the institute for Stem Cell Biology and Regenerative Medicine

Cell Biology & Regenerative Medicine
- Request Information
The PhD Graduate Program in Cell Biology & Regenerative Medicine (CBRM) provides students with the background, training, and experience necessary to launch a career as an independent scientific investigator that significantly contributes to the advancement of human health. Faculty in our research program use the tools of molecular and cellular biology, tissue engineering, genetic animal models, advanced imaging techniques, bioinformatics, and computational modeling to uncover novel therapeutic strategies to address musculoskeletal injuries, tissue repair and regeneration, cardiovascular diseases, fibrosis, vision disorders, mitochondrial diseases, neurodegenerative conditions, and more.
At a Glance
College of Life Sciences
Doctor of Philosophy
Center City
4 - 5 Years
The Cell Biology & Regenerative Medicine (CBRM) program is seeking students with a strong interest and background in science and engineering, particularly cell biology, developmental biology, molecular biology, biomedical engineering, bioengineering, biochemical engineering, quantitative biology, and related fields. Students are offered foundational coursework in their first year followed by a combination of electives tailored to their research interests and career aspirations. Students will develop competencies in tissue engineering, imaging for cell biology, bioinformatics, extracellular matrix biology and cell signaling. Formal training in grant proposal and scientific writing as well as weekly research discussion groups complete the student research and academic experience.
The CBRM program brings together faculty members across disciplines to offer students opportunities to craft their thesis research in a vibrant scientific environment with state-of the-art facilities. Students' research and education is fully supported through NIH training grants, endowed fellowships, investigator-initiated research grants, or individual graduate fellowships. The students also receive financial support to present their research findings at regional, national, and international scientific conferences. Graduates of the program have gone on to successful research careers in both academia and industry.
Here are the major research themes within the program:
- Musculoskeletal Biology
- Liver Disease, Surgery and Transplantation
- Cardiovascular Disease
- Mitochondrial Metabolism & Pathology
- Neurodegenerative & Vision Disorders
- Fibrosis & Matrix Biology
- Computational & Systems Biology
Additional Program Offerings
Get in touch, program director.
- Co-Director, Cell Biology & Regenerative Medicine PhD Program
- Associate Professor
Program Information
1020 Locust Street M-46 JAH Philadelphia , Pennsylvania 19107
Contact Admissions
- 215-951-2800
Connect with Us
- Graduate School
- Medical, health and life sciences
- Medical biotechnology
Regenerative medicine (including stem cells and tissue engineering)
Parent category, research centres, institutes & clusters in regenerative medicine (including stem cells and tissue engineering).
- BC Regenerative Medicine - BCRegMed
Graduate Degree Programs in Regenerative medicine (including stem cells and tissue engineering)
Master of engineering in biomedical engineering (meng).
Biomedical Engineers apply their knowledge in engineering, biology, and medicine to healthcare and medical device industries. Biomedical Engineering is a distinct field that encompasses engineering disciplines, biology, life sciences, medicine, clinical applications, and the improvement of human...
UBC Researchers conducting research in Regenerative medicine (including stem cells and tissue engineering)
Mcnagny, kelly marshall, school of biomedical engineering, department of medical genetics, faculty of medicine.
Faculty (G+PS eligible/member)
Cellular immunology; Regenerative medicine (including stem cells and tissue engineering); Stem Cells; Immunology; Inflammation; Mouse models of human disease; Tissue degeneration/regeneration; Cancer; innate immune response; kidney function; Biologics and therapeutics
Rana, MD Mohosin
Faculty of medicine.
Postdoctoral Fellow
Regenerative medicine (including stem cells and tissue engineering); Material Sciences; Polymer chemistry; Tissue Engineering; Organ Engineering; Nanotechnology; Regenerative medicine; microfluidics; Bioengineering
Wang, Rizhi
Department of materials engineering, school of biomedical engineering, faculty of applied science.
Functional materials in materials engineering sciences; Regenerative medicine (including stem cells and tissue engineering); Orthopaedic implants, drug delivery biomaterials, anti-infection solutions.; Additive manufacturing, 3D structural designing.; Bone structure, mineralization and mechanics, bone metastasis, hip fracture and prevention.
Student & Alumni Stories in Regenerative medicine (including stem cells and tissue engineering)

Tanya Bennet
Doctor of Philosophy in Biomedical Engineering (PhD)
Airway-On-A-Chip: Development and In Vitro Validation of a Microfluidic Cell Culture Model For Chronic Obstructive Pulmonary Disease

Omar Bashth
Uncovering the Role of Human Stem Cell Competition in Pluripotency and Lineage Commitment
Alexander Garner
Doctor of Philosophy in Cell and Developmental Biology (PhD)
Investigating how pancreatic islet architecture impacts function
Doctor of Philosophy in Experimental Medicine (PhD)
Mutations in the giant protein titin and risk of heart rhythm disorders

Saif Dababneh
Doctor of Medicine and Doctor of Philosophy (MDPhD)
Human stem cells and genomics to understand and treat heart rhythm disorders
French Name
French description, planning to do a research degree use our expert search to find a potential supervisor.
- Why Grad School at UBC?
- Graduate Degree Programs
- Application & Admission
- Info Sessions
- Research Supervisors
- Research Projects
- Indigenous Students
- International Students
- Tuition, Fees & Cost of Living
- Student Status & Classification
- Student Responsibilities
- Supervision
- Managing your Program
- Health, Wellbeing and Safety
- Professional Development
- Dissertation & Thesis Preparation
- Final Doctoral Exam
- Final Dissertation & Thesis Submission
- Life in Vancouver
- Vancouver Campus
- Graduate Student Spaces
- Graduate Life Centre
- Life as a Grad Student
- Graduate Student Ambassadors
- Meet our Students
- Award Opportunities
- Award Guidelines
- Minimum Funding Policy for PhD Students
- Killam Awards & Fellowships
- Dean's Message
- Leadership Team
- Strategic Plan & Priorities
- Vision & Mission
- Equity, Diversity & Inclusion
- Initiatives, Plans & Reports
- Graduate Education Analysis & Research
- Media Enquiries
- Newsletters
- Giving to Graduate Studies
Strategic Priorities
- Strategic Plan 2019-2024
- Improving Student Funding
- Promoting Excellence in Graduate Programs
- Enhancing Graduate Supervision
- Advancing Indigenous Inclusion
- Supporting Student Development and Success
- Reimagining Graduate Education
- Enriching the Student Experience
Initiatives
- Public Scholars Initiative
- 3 Minute Thesis (3MT)
- PhD Career Outcomes

Programme Overview
A 4 year funded integrated PhD and MSc in Tissue Engineering and Regenerative Medicine - Innovation in Medical and Biological Engineering.
Programme Structure
The CDT TERM iMBE is a blended programme of specialised subject modules, along with professional development and skills training, integrated with research over two years.
Our expertise is in the area of musculoskeletal and cardiovascular systems with our research focusing on three main areas - Joint Replacement, Tissue Re-engineering and Functional Spinal Intervention.
February 2020 CDT TERM Newsletter
The latest edition of the CDT TERM Newsletter Read all about the programme highlights, student progress and upcoming events CDT TERM Newsletter Feb 2020
Research Impact - Blog Launch
To demonstrate the impact of the EPSRC funded Centre for Doctoral Training in Tissue Engineering and Regenerative Medicine and also aligned PhD students at the University of Leeds we have launched a new blog which will showcase the research and development taking place to deliver regenerative therapies and devices which can repair or replace tissues and restore normal tissue function.
Leeds in top 40 most international universities
Leeds has been recognised as one of the world's most international universities. The Times Higher Education ranking shows that Leeds has risen for a second consecutive year, and is now in the top 40 in the world. Professor Hai-Sui Yu, the University of Leeds’ Deputy Vice-Chancellor: International, said: “Leeds attracts the brightest international students and scholars, harnessing great minds...
Tweet Your Thesis Conference - 2021
EPSRC CDT TERM at Leeds will be hosting a Thesis Twitter Conference on Wednesday 17th March 2021, 9am to 5pm. You can catch the action at CDTTERM-iMBE (@CDTTERMiMBE) / Twitter. The Thesis Twitter Conference provides a platform for you to engage an audience outside of your research field. It also allows you the opportunity to hone your skills in communicating your research concisely and clearly. Hopefully you will receive feedback and make new connections that you will maintain throughout your research career.
CDT Tissue Engineering and Regenerative Medicine - 2020 Careers Event
CDT Tissue Engineering and Regenerative Medicine - Careers Event Why attend? Develop your network, learn more about careers in different...
Cross CDT Poster Event 2020
12.30-13.30: CDT Year 2 students to display research posters 13.30-15.15: Poster Presentations, Judging & Light Refreshments 15.15-15.30: Presentation of Prizes
First Results
Finally, I can see a light at the end of the tunnel. The first three years of the PhD were very intense. As I predicted...
Adjusting after lockdown - Piers Wilkinson
As it probably goes without saying, the past several months has been a difficult period. Due to the pandemic the lab where I was based...
My PhD during lockdown - Valeria Filippou
As everyone, during the last few months I have had my ups and downs. I never imagined that the COVID situation could happen, however I...
Twitter Feed

Tissue Engineering and Regenerative Medicine
Investigating technologies from biomaterial/cell constructs for repairing various tissues and organs, to stem cell therapies, to immune therapies
Research in tissue engineering and regenerative medicine seeks to replace or regenerate diseased or damaged tissues, organs, and cells – a challenging endeavor, but one that has tremendous potential for the practice of medicine.
Technologies under investigation range from biomaterial/cell constructs for repairing various tissues and organs, to stem cell therapies, to immune therapies. Our work in this area is highly multidisciplinary, combining materials science, cell biology, clinical science, immunology, stem cell biology, genome science, and others.
Accordingly, researchers in this area within Duke BME are broadly interactive with departments throughout the university including Duke University Medical Center clinical departments, the Duke University School of Medicine departments of Cell Biology and Immunology, the Duke Department of Chemistry, and others. This community is also supported by centers and programs such as Regeneration Next and the Center for Biomolecular and Tissue Engineering (CBTE) .
Associated Faculty

Nenad Bursac, Ph.D.
Professor of Biomedical Engineering

Dr Pranam Chatterjee, Ph.D.
Assistant Professor of Biomedical Engineering

Joel Collier
Associate Dean for Doctoral Education, Theodore Kennedy Professor of BME

Sharon Gerecht
Chair of Biomedical Engineering, Paul M. Gross Distinguished Professor

Charlie Gersbach
John W. Strohbehn Distinguished Professor of Biomedical Engineering

John Hickey

Bruce Klitzman
Associate Professor Emeritus in Surgery

Samira Musah, Ph.D.
Assistant Professor in the Department of Biomedical Engineering

William M. Reichert
Professor Emeritus of Biomedical Engineering

Tatiana Segura

Cynthia Ann Toth
Joseph A.C. Wadsworth Distinguished Professor of Ophthalmology

George Truskey, Ph.D.
R. Eugene and Susie E. Goodson Distinguished Professor of Biomedical Engineering

Shyni Varghese
Laszlo Ormandy Distinguished Professor of Orthopaedic Surgery
Other Research Specialties
Explore additional specialty research areas in Duke BME and throughout the Pratt School of Engineering.
Postgraduate research
Stem cell & regenerative medicine phd / mphil / md.
- Part time available: yes
Studying in:
- institute-of-systems-molecular-and-integrative-biology
- Faculty of Health and Life Sciences
Regenerative Medicine is a multidisciplinary area of study covering stem cell biology, tissue engineering, bioengineering, chemical biology and gene therapy. This is a dynamic and growing area of research with the potential to advance diagnosis and treatment of disease, and improve the way patients are treated.
Why study with us?
Coming from a chemistry background I was initially worried about how well I would integrate into the ITM. However, the support from the ITM staff and students has been invaluable to my development. Niamh McCallum - Stem Cell & Regenerative Medicine PhD student
academic members of staff.
registered postgraduate research students.
A leading international centre for research into the fundamental principles of human physiology. We have recognised expertise in all aspects of modern physiology ranging from the regulation of gene expression to cell, tissue and whole organism biology.
This area of physiology research, utilises state-of-art technologies that enable non-invasive assessment of anatomy and function (MRI), protein expression and reporter gene expression (optical imaging), measurement of blood flow and vascularity (ultrasound) and renal function (photo-acoustic imaging). All have widespread applications for diagnostics and therapeutic interventions in neurology, neurosurgery, oncology, physiology, musculoskeletal biology and other relevant fields.
Research is undertaken within the Department of Cellular and Molecular Physiology, an integral part of the Institute for Translational Medicine.
This interdisciplinary research area is dedicated to harnessing the curative potential of stem cells to improve human health, with the central aim to bring life changing stem cell therapies closer to reality. Research is undertaken within the Department of Cellular and Molecular Physiology, an integral part of the Institute for Translational Medicine. Research spans from stem cell biology to tissue engineering to chemical biology with a focus on translational research. There are strong links to The Centre for Preclinical Imaging also within the Department of Cellular and Molecular Physiology, which provides expertise and infrastructure for non-invasive imaging in pre-clinical models. Linked to the UK Regenerative Medicine Platform. The UKRMP Safety and Efficacy Hub, led from Liverpool, is developing novel strategies for evaluating the safety and efficacy of regenerative medicine therapies, so that these important new medicines can be developed with full confidence.
Our research interests closely match our research themes.
Research themes
Research areas specifically focus on:
- Cellular and molecular based regenerative medicine therapies that can treat patients in the early stages of kidney disease, and help to prevent them from developing life threatening end stage kidney disease
- Developing more sensitive and specific methods to detect changes in chronic and acute liver disease earlier and to prevent irreversible liver failure
- Studying the intestinal epithelium to develop both cellular and molecular therapeutics that will stimulate the rapid regeneration of the intestinal epithelium, following intestinal barrier breakdown, as seen in inflammatory bowel disease
- Examining the enteric nervous system, for example researching potential treatments for Hirschsprung's disease, a condition resulting from the congenital absence of ENS ganglion cells in the gut.
PhD students can take taught modules - on either a formal basis with exams taken and a record of completion generated or less formally. Commonly, students use the opportunity to upskill in areas like bioinformatics and statistics, but modules on defined areas of biology are also available. A wide variety of further development opportunities are available from the PGR Development Hub .
The research infrastructure of the Institute of Translational Medicine is designed to give researchers access to world class facilities in the best possible environment.
Our centres, facilities and resources give us the ability to drive biomedical research from patient samples to the laboratory bench and vice versa from newly generated drug compounds into clinical trials. They provide powerful, productive collaborations between experts within the University and organisations worldwide.
- Biomedical Imaging
- Centre for Antimicrobial Pharmacodynamics
- Centre for Drug Safety Science
- Health Data Science Network
- Centre for Preclinical Imaging
- Clinical Trials Research Centre
- Harris-Wellbeing Preterm Birth Research Centre
- Liverpool Bio-Innovation Hub (LBIH) Biobank
- Liverpool Cancer Trials Unit
- MRC North West Hub for Trials Methodology Research
- North West Cancer Research Centre – University of Liverpool
- Pancreas Biomedical Research Unit
- UK Experimental Arthritis Treatment Centre for Children
- Wolfson Centre for Personalised Medicine.
Postgraduate researchers also benefit from flexible access to world-class equipment and expertise through the Shared Research Facilities provided.
Research groups
Regenerative Medicine Network
The Centre for Preclinical Imaging
Safety and Efficacy Hub
Study options and fees
The fees below reflect one year of study. Fees stated for UK students are for the academic year 2024/25 and are subject to change for 2025/26. Fees stated for international students are for the academic year 2025/25.
The fees stated in the table above exclude potential research support fees also known as ‘bench fees’. You will be notified of any fee which may apply in your offer letter.
* Please note that if you are undertaking a PhD within the Faculty of Science and Engineering the fee you pay, Band A or Band B, will reflect the nature of your research project. Some research projects incur a higher fee than others e.g. if you are required to undertake laboratory work. You will be informed of the fee for your programme in your offer letter.
Entry requirements
Applicants for postgraduate research study at Liverpool are normally expected to hold a UK first degree with a First Class or Upper Second Class degree classification, or a Second Class degree plus a Master’s degree. Equivalent international qualifications are also accepted, and their equivalence will be evaluated on the basis of the information provided by the National Academic Recognition and Information Centre (NARIC) as well as internal guidance based on our experience of a qualification’s suitability as a preparation for our programmes.
English language requirements
How to apply.
Research degree applications can be made online. You'll also need to ensure that you have funding to cover all fees.
Applications are open all year round .
More about applying for research degrees
Apply online
Before you apply, we recommend that you identify a supervisor and develop a research proposal
Find a supervisor
View staff list
Need help finding a supervisor? Contact us
- ISMIB PGR Administrator
- Email: [email protected]
- Phone: +44 (0)151 794 5455
Related studentships: self-funded and funded PhD projects
Related doctoral training partnerships.
Doctoral Training Partnerships support future researchers with funding and a rewarding learning environment where you can collaborate with leading researchers.
- MRC DiMeN Doctoral Training Partnership
- University of Liverpool Doctoral Network in Technologies for Healthy Ageing
Find a scholarship
We offer a range of scholarships to help you meet the costs of studying a research degree.
See scholarships

DEPARTMENT OF TISSUE ENGINEERING & REGENERATIVE MEDICINE, FACULTY OF MEDICINE
Doctor of philosophy (tissue engineering).

PhD (Tissue Engineering) aim to provide a platform for the postgraduate student to perform research and develop therapies to repair the impaired tissue and restore its normal function using regenerative medicine approaches, especially tissue engineering.
Tissue Engineering is a rapidly expanding field for application in regenerative medicine, which seeks to improve, replace or regenerate the repaired or damaged tissues and organs in humans. It is a multidisciplinary field that require the assimilation of knowledge from biology, chemistry and engineering. Recent development in the area of regenerative medicine has brought much anticipation of its application in medical and healthcare arena in very near future. This program will enable the students, together with their supervisors, to identify the needs in clinical setting and then, to formulate and develop a solution for the problem using tissue engineering applications. The program conducted at
Department of Tissue Engineering and Regenerative Research (DTERM), UKM will provide the students with interdisciplinary expert line-up, tissue-engineering laboratories equipped with excellent equipments, access to latest R&D technologies in the field, and an opportunity to collaborate with international academics. This course provides immediate career opportunity in the broad field of regenerative medicine.
- Meet all the postgraduate admission requirements set by UKM (refer to UKM postgraduate website)
- Masters degree in biology or related subjects (e.g. biology, biochemistry, biomedicine, biomedical engineering, material science etc.) from a recognized University
- Passed the interview by faculties at the Department of Tissue Engineering and Regenerative Medicine
Full time: 6-10 Semesters; Part time: 10-14 Semesters. Application and enrolment for PhD (Tissue Engineering) open throughout the year
The program involves research work in laboratory. The program is designed to train the student to scientifically study and report the findings in a research topic in the tissue-engineering field. Candidates will be guided and supervised by the faculties at the Centre for Tissue Engineering and Regenerative Medicine. Induction course upon entry to the program, scheduled weekly scientific meetings and other seminars and workshops will be the platform to gain and share knowledge in the area of tissue engineering. The student need to write up the research report in the form of thesis that will be examined and present it in other form of scientific communications such as journals and conference presentations.
For any inquiries about the course, email us at: [email protected]
For more information regarding registration and tuition fee, visit:.

DEPARTMENT OF TISSUE ENGINEERING & REGENERATIVE MEDICINE (DTERM)
Admin Office: 15th Floor, Pre-Clinical Building, Jalan Yaacob Latif, Bandar Tun Razak, 56000 Cheras, Kuala Lumpur, MALAYSIA.
Operational Office: 12th Floor, Blok Klinikal HCTM, Jalan Yaacob Latif, Bandar Tun Razak, 56000 Cheras, Kuala Lumpur, MALAYSIA.
Phone: +6 03 9145 6239 Email: [email protected]
VISIT US AT:
OPEN POSITION: Rice Bioengineering invites applications for Tenure-Track Assistant Professor. Click here to apply

KEY APPLICATION AREA
Tissue Engineering & Regenerative Medicine
Research in tissue engineering and regenerative medicine encompasses all aspects of the research and development continuum from mechanistic studies to translational approaches. Collaborative efforts with colleagues at Rice and the Texas Medical Center address unmet clinical needs for a plethora of tissues ranging from bone to cartilage to heart valve to inner ear.
Specific areas of interest include structure and function relationships in living tissues, synthesis and fabrication of biomimetic materials and extracellular matrix constructs, combinations of biomaterials with cell populations for modulating cell function and guiding tissue growth, stem cell programming, drug and gene delivery systems for tissue induction and regeneration, 3D printing and bioprinting, and bioreactor designs for cell culture and disease modeling.
Rice BIOE researchers working in this key application area:
Caleb bashor, phd, faculty profile | laboratory website, jane grande-allen, phd, isaac hilton, phd, kevin mchugh, phd, antonios mikos, phd, jordan miller, phd, robert raphael, phd, omid veiseh, phd.
Song Li, Ph.D.
- Chancellor’s Professor, Bioengineering
- Professor, Medicine
Song Li, Ph.D., integrates principles of engineering, biomaterials and mechanobiology to advance cell and tissue engineering methods. He seeks to develop stem cell-based methods to promote regeneration in the heart and neuromuscular system and to advance immunoengineering approaches to treat cancer and other diseases.
Li stands at the forefront of mechano-epigenetic engineering of cell fate, leveraging his expertise to engineer biomaterials and microdevices that effectively guide stem cell differentiation, cell reprogramming and immune cell functionalities. He has demonstrated innovation in fabricating tissue grafts and designing drug delivery platforms to facilitate the regeneration of tissues and organs such as the heart, blood vessels, spinal cord, peripheral nerves and muscles.
Li aims to develop more efficient and precise methods to reprogram cells into induced pluripotent stem cells, and investigates the physical and chemical activities in the stem cell microenvironment that regulate differentiation processes. With this information, he hopes to mimic stem cells’ natural environments by developing physical platforms that can influence reprogramming .
Li seeks to improve immune cell memory to effectively combat infectious diseases and cancer, and is exploring novel methods to manipulate immune cells to promote tissue regeneration and develop therapeutics for diseases such as diabetes.
“Cell reprogramming is one of the most exciting advancements in biotechnology in the past 20 years. It’s the cellular equivalent of wiping your computer’s memory clean and replacing it with new software. This is a very powerful process that could lead to therapies based on patients’ own cells and their own genes.”
Research Projects
- Controlling cell fate and functions through stem cell differentiation The process by which stem cells transform into specific, specialized cell types with distinct functions and features. differentiation The process by which stem cells transform into specific, specialized cell types with distinct functions and features. , cell reprogramming In stem cell research, scientists can reprogram cells that have undergone differentiation, such as skin or blood cells, to revert back into an embryonic-like state. The resulting cells are called induced pluripotent stem cells. reprogramming In stem cell research, scientists can reprogram cells that have undergone differentiation, such as skin or blood cells, to revert back into an embryonic-like state. The resulting cells are called induced pluripotent stem cells. and synthetic biology to inform regenerative medicine A field focused on developing and applying new therapies and techniques to repair, replace or regenerate tissues and organs and restore function that has been lost due to aging, disease, injury or genetic defects. regenerative medicine A field focused on developing and applying new therapies and techniques to repair, replace or regenerate tissues and organs and restore function that has been lost due to aging, disease, injury or genetic defects. advancements
- Understanding how physical factors regulate chromatin organization and induce epigenetic changes
- Developing mechano-epigenetic engineering approaches to control cell fate and rejuvenate aging stem cells Cells that have the ability to differentiate into multiple types of cells and make an unlimited number of copies of themselves. stem cells Cells that have the ability to differentiate into multiple types of cells and make an unlimited number of copies of themselves.
- Integrating mechanical, chemical and biological factors to engineer immune cells for stem cell-derived therapies
- Designing drug delivery systems to modulate immune cells, enhancing vaccine efficacy, achieving immune tolerance and promoting tissue regeneration
- Developing microdevices for in vivo A process, procedure or study performed on or in a living organism. in vivo A process, procedure or study performed on or in a living organism. monitoring and stimulation of immune cell activity
- Exploring the potential of electrical modulation as a method to promote neuromuscular regeneration
Post-doctoral fellowship
- Bioengineering, UC San Diego, 1998
- Ph.D., Bioengineering, UC San Diego, 1997
Related News

Min Lee , Ph.D.
- (310) 825-6674
UCLA School of Dentistry 10833 Le Conte Ave. Box 951668 Los Angeles, CA 90095-1668
- Full-Time Faculty
- Biosystems and Function
Min Lee, Ph.D. is a Professor in the Section of Biosystems and Function in the Division of Oral and Systemic Health Sciences at the UCLA School of Dentistry. His primary research area is to design and develop new biomaterial systems to provide fundamental bases and translational approaches to tissue engineering and regenerative medicine, particularly focusing on orthobiologics, material-based therapeutics to repair craniofacial and orthopedic skeletal defects, novel liposomal platform for drug and gene delivery, photopolymerizable hydrogel systems.
- Fan J, Lee CS, Kim S, Zhang X, Pi-Anfruns J, Guo M, Chen C, Rahnama M, Li J, Wu BM, Aghaloo T, Lee M.Trb3 controls mesenchymal stem cell lineage fate and enhances bone regeneration by scaffold-mediated local gene delivery. Biomaterials 264:120445, 2020.PMID: 33069136
- Lee CS, Hwang HS,Kim S, Fan J, Aghaloo T,Lee M.Inspired by nature: facile design of nanoclay-organic hydrogel bone sealant with multifunctional properties for robust bone regeneration. Advanced Functional Materials 30(43):2003717, 2020. PMCID:PMC759110
- Fan J, Lee CS, Kim S, Chen C, Aghaloo T, Lee M.Generation of small RNA-modulated exosome mimetics for bone regeneration. ACS Nano 14(9):11973-11984, 2020. PMCID:PMC7530137
- Lee CS, Kim S, Fan J, Hwang HS, Aghaloo T,Lee M.Smoothened agonist sterosome immobilized hybrid scaffold forbone regeneration. Science Advances 6(17):eaaz7822, 2020. PMCID:PMC7176430
- Zhang X, Fan J, Lee CS, Kim S, Chen C, Aghaloo T,Lee M.Apatite-binding nanoparticulate agonist of hedgehog signaling for bone repair. Advanced Functional Materials 30(12):1909218, 2020. PMCID:PMC7494204
- Cui Z, Kim S, Baljon J, Wu B, Aghaloo T, Lee M. Microporous chitosan-montmorillonite nanocomposite hydrogel for bone tissue engineering. Nature Communications 10(1):3523, 2019. PMCID:PMC6684526
Courses taught at UCLA:
- RFE102, Dental Materials (Course Chair)
- RFE400, Advanced Materials and Biomechanics (Course Chair)
- RFE104, Direct Restoration (Guest Lecturer)
- RFE202, Direct Restoration (Guest Lecturer)
- RFE207, Direct Restoration (Guest Lecturer)
- B.S., Yonsei University, Seoul, Korea, Materials Science and Engineering, 1997
- M.S., Yonsei University, Seoul, Korea, Materials Science and Engineering, 1999
- Ph.D., University of California, Los Angeles, CA, Biomedical Engineering, 2007
Material-based therapy to repair craniofacial defects
New biomolecular strategy to regulate adipo-osteogenic balance
Nanomaterials for drug and gene delivery
Exosome-based nanoplatform for targeted delivery
Injectable hydrogel system
Research Description:
Research in the Lee groupÊfocuses on the development of biomimetic polymer systems for tissue regeneration and drug delivery applications. His research interests are:
New therapy for bone repair
Various pathophysiologic processes of aging, obesity and osteoporosis are associated with the dysregulation of the adipo-osteogenic differentiation of mesenchymal stem cells (MSCs). Regulating the lineage commitment of MSCs has increasingly attracted great attention in recent years. We developed novel biomolecular strategies that favor osteogenesis over adipogenesis by regulating expression of tribbles proteins. Completion of this study will identify new therapies for the treatment of various bone marrow related diseases and metabolic abnormalities as well as for application of MSCs in tissue engineering.
Nanomaterials for controlled release
Therapeutic efficacy of drug molecules is affected by delivery kinetics due to their intrinsic instability and rapid degradation in the body. Sterosomes are a novel class of liposomes formed from single-chain amphiphiles and high content of sterols, and presented significantly increased stability compared to conventional phospholipid liposomes. We developed a novel sterosome formulation that exerts specific tissue targeting and intrinsic therapeutic effects even without drug loading. This system suggests a promising delivery vector for drugs and therapeutic genes.
Hydrogel carrier system
Hydrogels derived from naturally occurring polymers are attractive matrices for tissue engineering by delivering precursor/stem cells or therapeutic agents into defect sites through a minimally invasive manner. We developed a hydrogel design strategy to better guide cellular behavior and tissue formation by creating injectable and self-healing polymer network with controlled porous structures and tunable degradability. This system may serve as versatile biomaterial platform for many applications, including therapeutic delivery, cell carriers, and regenerative medicine.
Research Grants:
NIH/NIDCR R01 DE027332, Principal Investigator, 2018-2023
- Tribbles homolog 3 and BMP-2 induced bone formation
DOD W81XWH-18-1-0337 , Principal Investigator, 2018-2021
- Development of smoothened agonist nonphospholipid liposomal nanoparticles for bone repair
MTF Biologics , Principal Investigator, 2018-2021
- Enhanced biological activity of demineralized bone matrix with noggin suppression in polymer matrices
NIH/NIAMS R01 AR070773 , Aaron James (PI), Min Lee (PI of subcontract), 2017-2022
- Direct and indirect contributions of perivascular stem cells to bone healing
- Google Scholar
- 2019 - Associate Editor, Journal of Biological Engineering
- 2010- Member, Academy of Osseointegration
- 2010- Member, American Association for Dental Research
- 2010- Member, International Association for Dental Research
- 2010- Member, Jonsson Comprehensive Cancer Center
- 2008- Member, Tissue Engineering & Regenerative Medicine International Society
- 2007- Member, Society for Biomaterials
Publications

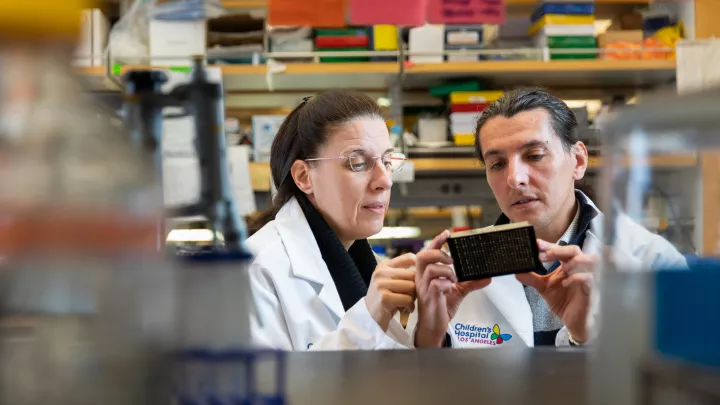
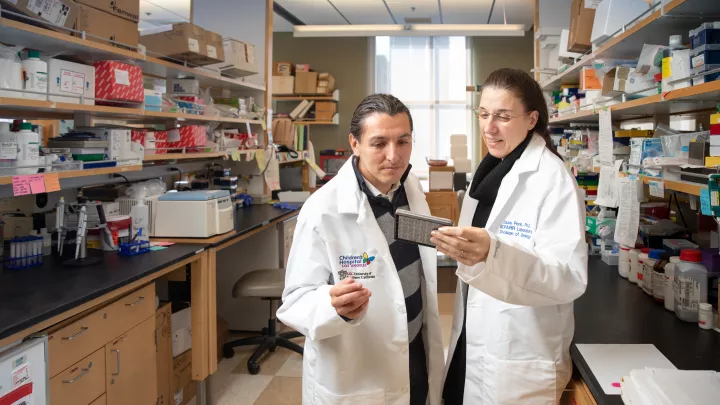
Astgik Petrosyan, PhD
Dr. Astgik Petrosyan‘s laboratory focuses on understanding the role of the extracellular matrix in cancer and development. She has expertise in tissue engineering, regenerative medicine, renal development, cancer, and chip technology.
University of Southern California, PhD, Development, Stem Cells, and Regenerative Medicine University of Southern California, Graduate Certificate, Diploma in Innovation
Accomplishments
American Society of Transplantation International Society for Stem Cell Research American Society of Nephrology Tissue Engineering and Regenerative Medicine International Society
Transplant Regenerative Medicine Committees of Practice (COP) Executive Committee Member at Large, American Society of Transplantation
Frank CN, Hou X, Petrosyan A , Villani V, Zhao R, Hansen JR, Clair G, Salem F, De Filippo RE, Cravedi P, Lemley KV, Perin L. Effect of disease progression on the podocyte cell cycle in Alport Syndrome . Kidney Int. 2022 Jan;101(1):106-118. PMID: 34562503.
Angeletti A, Cantarelli C, Petrosyan A , Andrighetto S, Budge K, D'Agati VD, Hartzell S, Malvi D, Donadei C, Thurman JM, Galešić-Ljubanović D, He JC, Xiao W, Campbell KN, Wong J, Fischman C, Manrique J, Zaza G, Fiaccadori E, La Manna G, Fribourg M, Leventhal J, Da Sacco S, Perin L, Heeger PS, Cravedi P. Loss of decay-accelerating factor triggers podocyte injury and glomerulosclerosis . J Exp Med. 2020 Sep 7;217(9):e20191699. PMID: 32717081.
Petrosyan A, Cravedi P, Villani V, Angeletti A, Manrique J, Renieri A, De Filippo RE, Perin L, Da Sacco S. A glomerulus-on-a-chip to recapitulate the human glomerular filtration barrier . Nat Commun. 2019 Aug 13;10(1):3656. PMID: 31409793.
Petrosyan A , Zanusso I, Lavarreda-Pearce M, Leslie S, Sedrakyan S, De Filippo RE, Orlando G, Da Sacco S, Perin L. Decellularized Renal Matrix and Regenerative Medicine of the Kidney: A Different Point of View . Tissue Eng Part B Rev. 2016, Jun;22(3):183-92. PMID: 26653996.
Petrosyan A , Da Sacco S, Tripuraneni N, Kreuser U, Lavarreda-Pearce M, Tamburrini R, De Filippo RE, Orlando G, Cravedi P, Perin L. A step towards clinical application of acellular matrix: A clue from macrophage polarization . Matrix Biol. 2017 Jan;57-58:334-346 PMID: 27575985.
Peloso A, Petrosyan A , Da Sacco S, Booth C, Zambon JP, OʼBrien T, Aardema C, Robertson J, De Filippo RE, Soker S, Stratta RJ, Perin L, Orlando G. Renal Extracellular Matrix Scaffolds From Discarded Kidneys Maintain Glomerular Morphometry and Vascular Resilience and Retains Critical Growth Factors. Transplantation . 2015 Sep;99(9):1807-16. PMID: 26018349.
Da Sacco S, Lemley KV, Sedrakyan S, Zanusso I, Petrosyan A, Peti-Peterdi J, Burford J, De Filippo RE, Perin L. A novel source of cultured podocytes . PLoS One. 2013 Dec 12;8(12):e81812. PMID: 24349133.
Stem Cells, Extracellular Matrix, Molecular Biology, Regenerative Medicine, Cancer, Glomerulus on a Chip, and Human Kidney Developmental Biology
Medical Xpress - Researchers uncover new clues to origins of the most common pediatric kidney cancer
Astgik Petrosyan, PhD News

Could a Key Protein Lead to New Therapies for Wilms Tumor?
Study Offers New Insights Into How the Most Common Kidney Cancer Starts in Kids
Children’s Hospital Los Angeles Researchers Uncover New Clues to Origins of the Most Common Pediatric Kidney Cancer

All Children’s Hospital Los Angeles locations are open.
Wildfire Support Line for Current Patients, Families and Team Members: 323-361-1121 (no texts) 8 a.m. - 7 p.m.
Stay Up to Date
Sign up to receive our monthly newsletter, latest news, events and stories delivered right to your inbox.
Brush Up: Tissue Engineering and Regenerative Medicine
A new frontier in repairing organ damage

View Full Profile .
Learn about our Editorial Policies .
What Is Regenerative Medicine? Regenerative medicine replaces tissue or organs that are damaged by trauma, disease, or congenital disorders. This is different from more traditional therapies that treat the symptoms of tissue damage. There are three main concentrations within the field of regenerative medicine: tissue engineering, cellular therapy, and artificial organs. The use of tissue engineering in regenerative medicine, known as TERM, is an active area of research that involves creating functional tissue through the combination of cells, scaffolds, and growth factors to restore normal biological function. 1 Clinicians treat millions of patients with tissue engineered regenerative devices. So far, the most successful tissue regeneration therapies occur in soft tissues such as skin, cartilage, and corneal tissues.
Using Tissue Engineering to Regenerate Damaged Tissue
How does tissue engineering work?
During healthy tissue development, cells build and surround themselves with an extracellular matrix. This matrix, or scaffold, contains structural proteins and acts as a reservoir for signaling molecules that cells use to communicate and organize themselves into functional complexes or tissues.
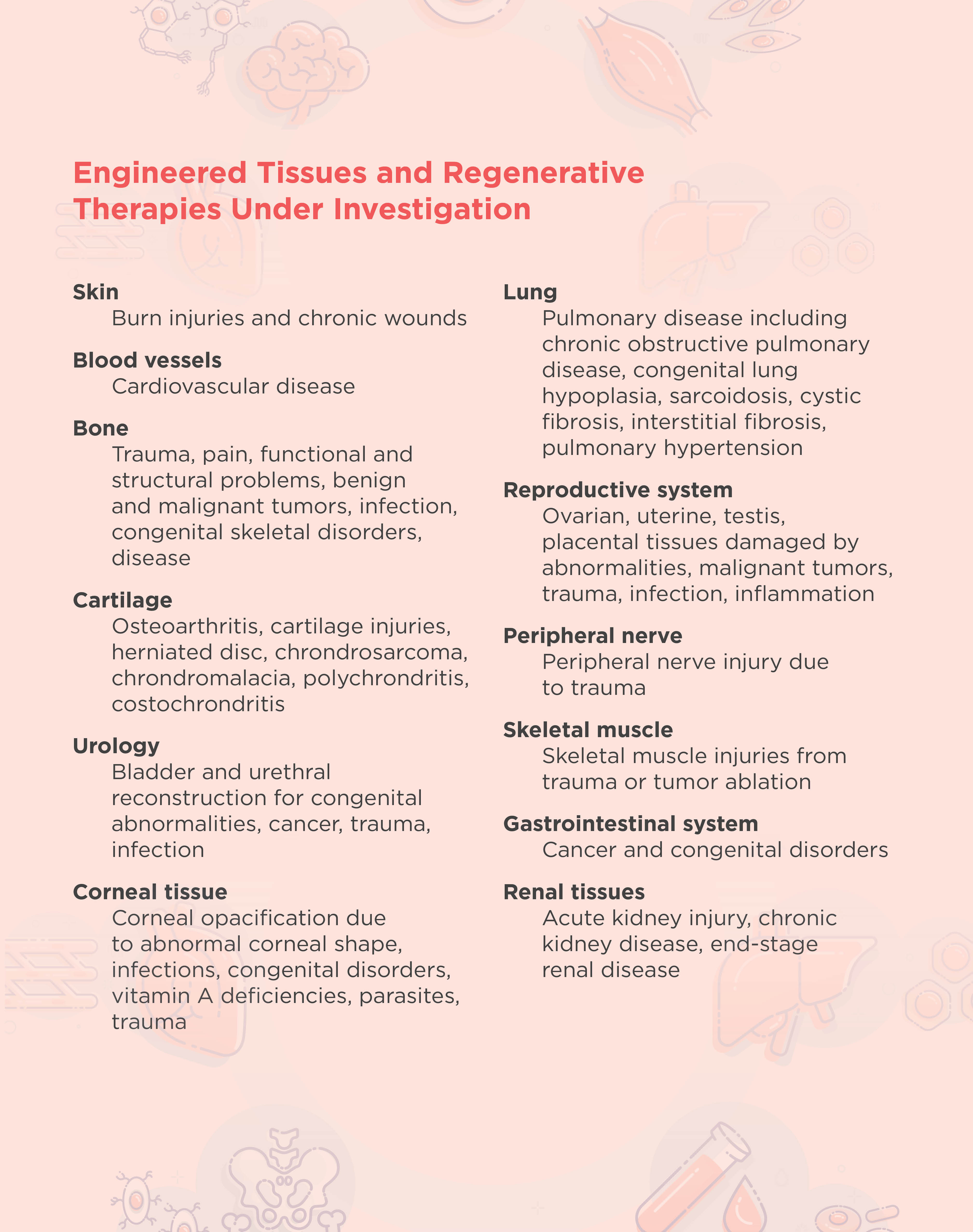
The overall goal of tissue engineering in the context of regenerative medicine is to establish a 3D cell or biomaterial complex that functions similarly to the in vivo tissue extracellular matrix. In general, tissue engineering involves the design and implantation of a scaffold that is biologically compatible with the area to be regenerated. New cells are then either attracted to or grown directly onto the scaffold. 2 The FDA has approved engineered artificial cartilage and skin therapies, and researchers are developing many other therapies for different tissues and disorders (see table below).
Scaffolds in tissue engineering Scientists seed scaffolds with their desired cell type during or following implantation. Alternatively, they may add growth factors to the scaffold and wait until the structure is populated by the surrounding tissue.
Choosing a scaffold type and source for tissue engineering is imperative for regenerating functional tissue. Pore size and overall architecture are important variables to consider when designing a scaffold. Pores play a crucial role in tissue regeneration because they allow for the exchange of nutrition and oxygen with surrounding tissue as well as expulsion of waste products and vascularization. The overall architecture of the tissue is important for exposing surfaces for cell attachment as well as mechanical cell stimuli.
Scaffolds can be natural or synthetic. Natural scaffolds are derived from donor tissues where the cells are chemically removed, leaving only the extracellular matrix. Natural scaffolds can either come from a patient or a healthy donor, and they have the advantage of retaining the unique structural and functional architecture of complex tissues. Researchers can also create natural scaffolds in vitro, such as those made from collagen and Matrigel, which are comprised of basement membrane proteins. 3,4
Scientists can develop synthetic scaffolds from various polymers, including polyglycolic acid (PGA), polylactic acid (PLA), and poly(lactide-co-glycolide) acid (PLGA). Scaffolds made with these polymers are flexible and porous, making them ideal structures for cellular integration. Synthetic scaffolds are also biodegradable, with different polymers degrading at different times, allowing damaged tissue to regenerate without the use of permanent prosthetic implants. Synthetic scaffolds also have consistent structures between replicates as they are generated in a laboratory; however, they can cause inflammation in the recipient more readily than natural scaffolds. 5
3D printing in tissue engineering With recent progress in 3D printing methods, researchers create complex synthetic scaffold structures with more consistent architecture and pore sizes. Hydrogel materials, such as alginate hydrogel and gelatin, are typically used in 3D printing due to their effective crosslinking and biocompatible properties. 6
Stem cells in tissue engineering and regenerative therapy Mesenchymal, embryonic, and induced pluripotent stem cells effectively promote damaged tissue regeneration. However, in many tissues, transplanted stem cells have poor survival and differentiation capabilities. The development of stem cell technology in combination with tissue engineering techniques, such as scaffolds and the addition of growth factors, has allowed researchers to improve the viability and proliferation of stem cells in regenerative medicine. 7
2. F. Han et al., “Tissue engineering and regenerative medicine: Achievements, future, and sustainability in Asia,” Front Bioeng Biotechnol , 8:83, 2020.
3. S. Sundaram et al., “Tissue engineering and regenerative medicine” in Rossi's Principles of Transfusion Medicine . Fifth edition. T.L. Simon, ed., New York, N.Y.: John Wiley & Sons Inc., 2016, pp. 488-504.
4. C. Motta et al., “Tissue engineering and regenerative medicine” in Rossi's Principles of Transfusion Medicine . Sixth edition. T.L. Simon, ed., New York, N.Y.: John Wiley & Sons Inc., 2022, pp. 648-660.
5. Y. Li et al., “The effect of mechanical loads on the degradation of aliphatic biodegradable polyesters,” Regen Biomater , 4:179-190, 2017.
6. Z. Yazdanpanah et al., “3D bioprinted scaffolds for bone tissue engineering: State-of-the-art and emerging technologies,” Front Bioeng Biotechnol , 10:824156, 2022.
7. S.G. Kwon et al., “Recent advances in stem cell therapeutics and tissue engineering strategies,” Biomater Res , 22:36, 2018.

- 3D printing ,
- Brush-up Summaries ,
- Cell & Molecular Biology ,
- regenerative medicine ,
- stem cell ,
- The Scientist University ,
- tissue engineering
Meet the Author

Jennifer Zieba, PhD

Why Do Some People Get Drunk Faster Than Others?
Genetics and tolerance shake up how alcohol affects each person, creating a unique cocktail of experiences.
Research Resources
Infographics.

Sex Differences in Neurological Research
Experts from the Women’s Brain Foundation and bit.bio will explore the importance of sex-specific in vitro models for neurological research and drug discovery.

New Frontiers in Vaccine Development
Discover how scientists are designing the next groundbreaking vaccines against infectious diseases.

New Approaches for Decoding Cancer at the Single-Cell Level
In this webinar, Linghua Wang and Jeremy Goecks will talk about technology that enables new approaches for a better understanding of tumors on a cellular, spatial, and environmental level.

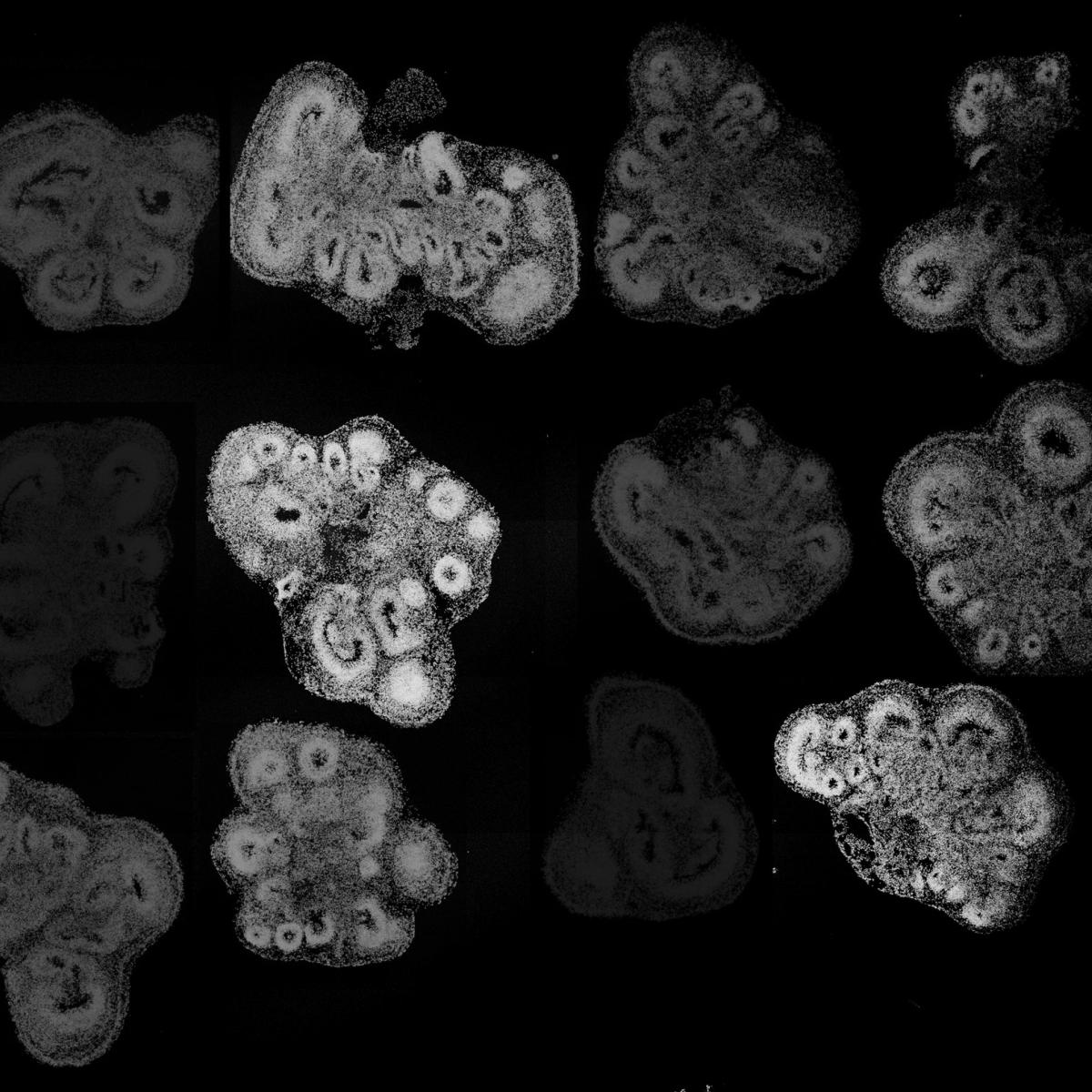
Organoids as a Tool for Tissue Regeneration Research
Explore how researchers use organoids to understand tissue regeneration and develop novel therapies.

Product News

Artificial Inc. proof-of-concept data demonstrates platform capabilities with NVIDIA’s BioNeMo
Collaborative project with world leader in AI computing demonstrates Artificial workflows and model integration for self-driving generative virtual screening in drug discovery. Company also announces key accreditations in recognition of excellence in data security, AI innovation, and commitment to continuous improvement.

Sapient Partners with Alamar Biosciences to Extend Targeted Proteomics Services Using NULISA™ Assays for Cytokines, Chemokines, and Inflammatory Mediators
Partnership complements Sapient’s mass spectrometry-based proteomics services, extends multi-omics solutions, and will enable development of NULISAseq™ assays under regulated guidance

Bio-Rad Extends Range of Vericheck ddPCR Empty-Full Capsid Kits to Optimize AAV Vector Characterization
Bio-Rad Laboratories, Inc. (NYSE: BIO and BIO.B), a global leader in life science research and clinical diagnostics products, today announced the launch of Vericheck ddPCR™ Empty-Full Capsid Kits for adeno-associated virus (AAV) serotypes 2 and 8, enabling determination of capsid titer, genome titer, and percentage of full capsids in purified or unpurified (crude lysate) samples.

Accelerating Mycoplasma Testing for Targeted Therapy Development
Tailored nucleic acid extraction and amplification methods help scientists overcome the challenges of detecting Mycoplasma contamination in advanced therapy medicinal products.

Biotech Pioneer Nina Tandon to Speak on Future of Regenerative Medicine

EpiBone CEO and co-founder Nina Tandon has earned distinction as one of the most creative people in business for her innovative research focused on studying electrical signaling in the context of tissue engineering.
Groundbreaking biotech leader Nina Tandon, PhD, will deliver a special address on the future of health technology and biology's industrial revolution Thursday, January 30, at 5:30 p.m. in the Hatfield Hall Theater. The event, which is free and open to the public, is being jointly presented by the Swearingen Leadership Series and the Rose Research Fellows Program . No advanced tickets are necessary. Seating is on a first-come, first-served basis.
Tandon is chief executive officer and co-founder of EpiBone, the world's first company to grow living human bone for skeletal reconstruction. Under her leadership, the company has achieved Federal Drug Administration approval for clinical trials of its revolutionary stem cell technology, which promises simplified surgery procedures, improved bone formation, and shorter recovery times for patients.
“Dr. Tandon is leading us into an exciting world where we could possibly create our own futures, using our own cells for our health and healing purposes,” said Associate Professor of Chemical Engineering Irene Reizman , PhD, creator of the Rose Research Fellows program, which is being supported by her term as the Alfred R. Schmidt Endowed Chair for Excellence in Teaching. “This will be an excellent opportunity for our students and others interested in science and scientific research from throughout the Wabash Valley to get insight about innovative biotechnology research from a pioneer in the field of cell biology.”
Tandon’s innovative research has focused on studying electrical signaling in the context of tissue engineering, and she has worked with cardiac, skin, bone, and neural tissue. This groundbreaking work in biomedical engineering has earned her recognition as one of Most Creative People in Business by Fast Company , an Innovation Fellow by WIRED , and a World Economic Forum Tech Pioneer. She co-authored “ Super Cells: Building with Biology ,” a book cataloguing the latest biotech inventions “using nature’s building block: the cell.”
The Swearingen Leadership Series brings speakers to campus to encourage development of future leaders in science, engineering, and mathematics to solve complex problems. It was established through support from John Swearingen, a 1981 Rose-Hulman chemical engineering alumnus, and his wife, Anne.
The Rose Research Fellows program introduces first- and second-year students opportunities to the fundamentals of research by completing a variety of projects, with faculty mentors, in science, engineering, and mathematics areas of interest. They also get opportunities to attend virtual and campus speaker events with Rose-Hulman alumni and other guests. Students then showcase their projects in a final formal presentation to the campus community at the end of the school year.
Unlocking new pathways in regenerative medicine
ASU's Harris Lab making strides toward tissue regeneration for wound healing, injury repair

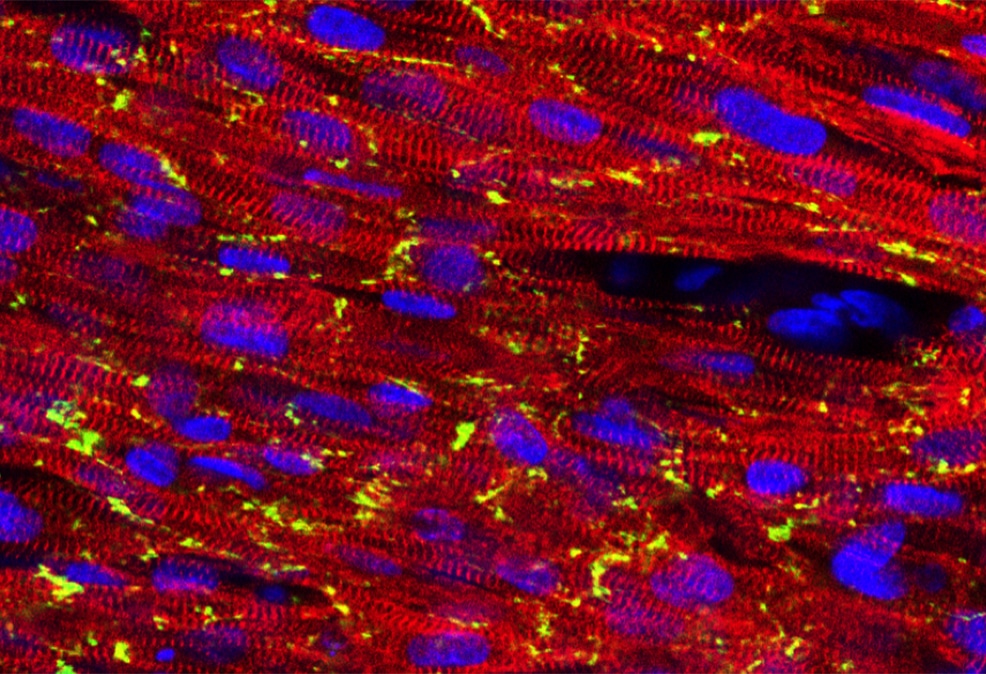
A fluorescent microscopy figure. Photo courtesy of Rob Harris
In the quest to advance regenerative medicine, the Harris Lab at Arizona State University is making groundbreaking strides. Focused on tissue regeneration and the intricate biology of cell death, the lab has uncovered a novel phenomenon with far-reaching implications for improving wound healing and injury repair.
This research not only fills a critical gap in our understanding of necrotic damage but also holds promise for developing innovative therapies for a wide range of medical conditions.
Led by Rob Harris , assistant professor in ASU's School of Life Sciences, the Harris Lab investigates how cells respond to necrotic damage — a poorly understood form of cell death caused by traumatic injuries, infections and common diseases such as heart attacks, strokes and diabetes. Necrosis, unlike the more controlled process of programmed cell death (apoptosis), often results in widespread tissue damage and inflammation. Understanding how tissues repair themselves in the aftermath of necrosis could transform treatment approaches for these conditions.
The Harris Lab employs the larvae of the common fruit fly (Drosophila melanogaster) as a model organism. While small and seemingly simple, fruit flies possess a surprising ability to regenerate damaged organs after various types of injuries, including physical trauma, irradiation and genetic disruptions. By leveraging this regenerative capacity, the lab is uncovering fundamental biological principles that could one day inform human therapies.
In their pivotal 2021 study published in Genetics, the Harris Lab identified an unexpected role for caspase proteins in tissue regeneration. Caspases are typically known for their involvement in apoptosis, wherein they help dismantle old or unwanted cells in a controlled manner. However, the lab’s research revealed something unexpected: Caspases activated by necrotic damage stimulate neighboring healthy cells to proliferate and contribute to tissue repair.
What’s even more remarkable is that this regenerative response occurs at a distance from the site of necrosis, suggesting the existence of long-range signaling mechanisms. These signals appear to mobilize surrounding healthy tissue to participate in the repair process, providing a more comprehensive response to injury.
“This finding is significant because it not only adds to the body of evidence that caspases are involved in signaling events that promote repair, but also shows for the first time that this phenomenon occurs following necrosis, one of the least understood and most prevalent forms of tissue damage in people,” Harris says.
This discovery not only challenges existing paradigms about the role of caspases but also expands our understanding of how tissues can coordinate their regeneration efforts after severe damage.
Building on these findings, the lab published a follow-up study in eLife last month. This research delves deeper into the molecular pathways underlying the observed phenomenon, providing new insights into how tissues achieve regenerative competence. By mapping the signaling events that link necrotic damage to caspase activation and subsequent cell proliferation, the lab has created a foundation for further exploration of these processes.
The significance of this work has not gone unnoticed. Andreas Bergmann, a renowned expert in cell death and tissue regeneration at UMass Chan Medical School, authored an eLife Insight article highlighting the groundbreaking nature of the Harris Lab’s discoveries. In his article, Bergmann notes, “By understanding the factors that confer regenerative competence to specific regions of the tissue, new fundamental principles of tissue regeneration may be uncovered. These insights could potentially be leveraged to develop novel therapeutic approaches for enhancing regenerative capacity in human tissues affected by necrotic damage.”
See what it's like to be an undergraduate researcher in the Harris Lab:
More Science and technology

Decades of data show age plays an important role in primate reproduction
There are a lot of factors that affect whether a baby gelada monkey or chacma baboon survives its first year of life, including a mother’s experience, food sources and infanticide. Recently,…

ASU, AAAS launch collaborative to strengthen scientific advancements
Today, the American Association for the Advancement of Science and Arizona State University announced a five-year partnership, the AAAS + ASU Collaborative. Together, the institutions will…
Scientists discover unique microbes in Amazonian peatlands that could influence climate change
Complex organisms, thousands of times smaller than a grain of sand, can shape massive ecosystems and influence the fate of Earth's climate, according to a new study.Researchers from Arizona State…
UC Irvine-led discovery of new skeletal tissue advances regenerative medicine potential
‘Lipocartilage’ properties akin to bubbled packaging material – super-stable, soft, springy

Irvine, Calif., Jan. 9, 2025 — An international research team led by the University of California, Irvine has discovered a new type of skeletal tissue that offers great potential for advancing regenerative medicine and tissue engineering.
Most cartilage relies on an external extracellular matrix for strength, but “lipocartilage,” which is found in the ears, nose and throat of mammals, is uniquely packed with fat-filled cells called “lipochondrocytes” that provide super-stable internal support, enabling the tissue to remain soft and springy – similar to bubbled packaging material.
The study , published online today in the journal Science , describes how lipocartilage cells create and maintain their own lipid reservoirs, remaining constant in size. Unlike ordinary adipocyte fat cells, lipochondrocytes never shrink or expand in response to food availability.
“Lipocartilage’s resilience and stability provide a compliant, elastic quality that’s perfect for flexible body parts such as earlobes or the tip of the nose, opening exciting possibilities in regenerative medicine and tissue engineering, particularly for facial defects or injuries,” said corresponding author Maksim Plikus, UC Irvine professor of developmental and cell biology. “Currently, cartilage reconstruction often requires harvesting tissue from the patient’s rib – a painful and invasive procedure. In the future, patient-specific lipochondrocytes could be derived from stem cells, purified and used to manufacture living cartilage tailored to individual needs. With the help of 3D printing, these engineered tissues could be shaped to fit precisely, offering new solutions for treating birth defects, trauma and various cartilage diseases.”

Dr. Franz Leydig first recognized lipochondrocytes in 1854, when he noted the presence of fat droplets in the cartilage of rat ears, a finding that was largely forgotten until now. With modern biochemical tools and advanced imaging methods, UC Irvine researchers comprehensively characterized lipocartilage’s molecular biology, metabolism and structural role in skeletal tissues.
They also uncovered the genetic process that suppresses the activity of enzymes that break down fats and reduce the absorption of new fat molecules, effectively locking lipochondrocytes’s lipid reserves in place. When stripped of its lipids, the lipocartilage becomes stiff and brittle, highlighting the importance of its fat-filled cells in maintaining the tissue’s combination of durability and flexibility. In addition, the team noted that in some mammals, such as bats, lipochondrocytes assemble into intricate shapes, like parallel ridges in their oversized ears, which may enhance hearing acuity by modulating sound waves.
“The discovery of the unique lipid biology of lipocartilage challenges long-standing assumptions in biomechanics and opens doors to countless research opportunities,” said the study’s lead author, Raul Ramos, a postdoctoral researcher in the Plikus laboratory for developmental and regenerative biology. “Future directions include gaining an understanding of how lipochondrocytes maintain their stability over time and the molecular programs that govern their form and function, as well as insights into the mechanisms of cellular aging. Our findings underscore the versatility of lipids beyond metabolism and suggest new ways to harness their properties in tissue engineering and medicine.”
The team included healthcare professionals and academics from the U.S., Australia, Belarus, Denmark, Germany, Japan, South Korea and Singapore, as well as staff from the Serrano Animal & Bird Hospital in Lake Forest and the Santa Ana Zoo. See the full list here.
This work was supported in part by the W.M. Keck Foundation under grant WMKF-5634988; UCI Beall Applied Innovation under Proof of Product grant IR-PR57179; LEO Foundation grants LF-AW-RAM-19-400008 and LF-OC-20-000611; Chan Zuckerberg Initiative grant AN-0000000062; Horizon Europe grant 101137006; National Institutes of Health grants U01-AR073159, R01- AR079470, R01-AR079150, R21-AR078939, P30-AR075047, R01-AR078389-01, R01-DE015038, R01-AR071457, R01-AR067821, R01GM152494, R01DE030565, TL1-TR001415, R01-DE013828, R01- DE30565, R01-HD073182, R01-AR067797, R01-DE017914 and MBRS-IMSD training grant GM055246; National Science Foundation grants DMS1951144, IOS-2421118, DMS1763272, CBET2134916, NSF-GRFP DGE-1321846 and MCB 2028424. Additional backing came from Simons Foundation grant 594598, the Yoshida Scholarship Foundation, a Howard A. Scheiderman Fellowship Award, the Ben F. Love Chair in Cancer Research at Baylor College of Medicine, the UC Riverside School of Medicine Dean’s Postdoc to Faculty Program and the Danish Cancer Society.
About UC Irvine’s Brilliant Future campaign: Publicly launched on Oct. 4, 2019, the Brilliant Future campaign aims to raise awareness and support for UC Irvine. By engaging 75,000 alumni and garnering $2 billion in philanthropic investment, UC Irvine seeks to reach new heights of excellence in student success, health and wellness, research and more. The Charlie Dunlop School of Biological Sciences plays a vital role in the success of the campaign. Learn more by visiting https://brilliantfuture.uci.edu/school-of-biological-sciences .
About the University of California, Irvine: Founded in 1965, UC Irvine is a member of the prestigious Association of American Universities and is ranked among the nation’s top 10 public universities by U.S. News & World Report . The campus has produced five Nobel laureates and is known for its academic achievement, premier research, innovation and anteater mascot. Led by Chancellor Howard Gillman, UC Irvine has more than 36,000 students and offers 224 degree programs. It’s located in one of the world’s safest and most economically vibrant communities and is Orange County’s second-largest employer, contributing $7 billion annually to the local economy and $8 billion statewide. For more on UC Irvine, visit www.uci.edu .
Media access: Radio programs/stations may, for a fee, use an on-campus studio with a Comrex IP audio codec to interview UC Irvine faculty and experts, subject to availability and university approval. For more UC Irvine news, visit news.uci.edu . Additional resources for journalists may be found at https://news.uci.edu/media-resources .
- Engineering (L1)
- Biomedical Engineering (L2)
- Tissue Engineering (L3)
Bladder Tissue Engineering and Regeneration
Bladder tissue engineering and regeneration is an emerging field focused on developing innovative solutions for bladder repair and reconstruction, particularly in patients with bladder dysfunction or damage due to conditions such as cancer or congenital abnormalities. Traditional surgical methods often involve using autologous tissue, which can lead to complications and a decrease in the patient's quality of life. Recent research has explored various bioengineered materials and techniques to create scaffolds that can support bladder tissue regeneration while minimizing the risks associated with conventional surgeries.
Recent Research
One significant area of research involves the use of decellularized tissues as scaffolds for bladder reconstruction. For instance, a study demonstrated the potential of porcine small intestinal submucosa (SIS) as a scaffold for creating a tissue-engineered urinary conduit. This approach aims to replace the need for autologous intestinal segments, which are commonly used in urinary diversions after bladder removal due to cancer. The study highlighted a novel decellularization process that effectively removes cellular material while preserving the extracellular matrix, making SIS a promising candidate for urinary diversion applications[1].
In pediatric urology, tissue engineering is being explored to address congenital conditions affecting the urethra and bladder. Traditional surgical procedures, such as urethroplasty and enterocystoplasty, are associated with significant complications. Research has focused on various biomaterials and strategies to enhance tissue regeneration, particularly in children, where the availability of suitable autologous tissue can be limited. The review emphasized the importance of combining seeded cells and growth factors with scaffolds to improve outcomes in urethral and bladder reconstruction[2].
Another innovative approach involves the use of adipose-derived stem cells (ASCs) in conjunction with bladder acellular matrix (BAM) for bladder augmentation. A study showed that scaffolds prepared with ASCs promoted better regeneration of bladder wall structures compared to unseeded scaffolds. This method demonstrated improved physiological function and structural integrity, indicating that combining stem cells with engineered scaffolds could enhance bladder tissue regeneration[3].
Additionally, researchers are developing decellularized extracellular matrices (dECMs) that are resistant to enzymatic degradation and compliant with bladder tissue. These modified dECMs have shown promising results in preclinical models, supporting the regeneration of bladder structures while reducing complications such as calculi formation. The enhanced properties of these materials suggest they could be effective in urologic tissue regeneration applications[4].
Technical Terms
Decellularization: A process that removes cells from a tissue or organ, leaving behind the extracellular matrix, which can be used as a scaffold for tissue engineering.
Extracellular Matrix (ECM): A complex network of proteins and carbohydrates that provide structural and biochemical support to surrounding cells.
Adipose-Derived Stem Cells (ASCs): Stem cells obtained from adipose (fat) tissue that have the potential to differentiate into various cell types, including those needed for tissue regeneration.
Urothelium: The epithelial lining of the bladder that plays a crucial role in bladder function and protection against urine.
- Porcine Small Intestinal Submucosa (SIS) as a Suitable Scaffold for the Creation of a Tissue-Engineered Urinary Conduit: Decellularization, Biomechanical and Biocompatibility Characterization Using New Approaches
- Tissue Engineering and Regenerative Medicine in Pediatric Urology: Urethral and Urinary Bladder Reconstruction
- Bladder Acellular Matrix Prepared by a Self-Designed Perfusion System and Adipose-Derived Stem Cells to Promote Bladder Tissue Regeneration
- Development of Enzymatic-Resistant and Compliant Decellularized Extracellular Matrixes via Aliphatic Chain Modification for Bladder Tissue Engineering
Learn more about Nature’s comprehensive data sources

IMAGES
COMMENTS
Regenerative medicine is transforming clinical practice with the development of new therapies, treatments and surgeries for patients with chronic conditions, debilitating injuries and degenerative diseases.
Graduate Program in Stem Cell Biology & Regenerative Medicine Stanford is a world leader in stem cell research and regenerative medicine. Central discoveries in stem cell biology – tissue stem cells and their use for regenerative therapies, transdifferentiation into mature cell-types, isolation of cancerous stem cells, and stem cell signaling ...
Jan 5, 2019 · Interested in exploring the untapped potential of stem cells in tissue regeneration and healing using cutting-edge interdisciplinary research techniques?. Read more. Tissue engineering and regenerative medicine approaches to understand and treat eye disease.
6 days ago · The PhD track in Tissue Engineering and Regenerative Medicine (TERM) prepares the students for a career in cutting edge research and development of cell- and biomaterial-based medical products.
The PhD Graduate Program in Cell Biology & Regenerative Medicine (CBRM) provides students with the background, training, and experience necessary to launch a career as an independent scientific investigator that significantly contributes to the advancement of human health. Faculty in our research program use the tools of molecular and cellular ...
Tissue engineering and regenerative medicine approaches to understand and treat eye disease.
This subclass comprises research and experimental development in regenerative medicine (including stem cells and tissue engineering).
The programme includes an integrated MSc in Tissue Engineering and Regenerative Medicine which comprises of compulsory and optional taught modules over the first two years with the majority studied in year 1, allowing a phased increase to full time research towards the end of year 2.
Nov 4, 2020 · A 4 year funded integrated PhD and MSc in Tissue Engineering and Regenerative Medicine - Innovation in Medical and Biological Engineering.
Research in tissue engineering and regenerative medicine seeks to replace or regenerate diseased or damaged tissues, organs, and cells – a challenging endeavor, but one that has tremendous potential for the practice of medicine.
The Tissue Engineering and Regenerative Medicine PhD/MSc programme from University of Leeds comprise of a blended programme of specialised subject modules, along with professional development and skills training, integrated with research over two years.
Regenerative Medicine is a multidisciplinary area of study covering stem cell biology, tissue engineering, bioengineering, chemical biology and gene therapy. This is a dynamic and growing area of research with the potential to advance diagnosis and treatment of disease, and improve the way patients are treated. \n
PhD (Tissue Engineering) aim to provide a platform for the postgraduate student to perform research and develop therapies to repair the impaired tissue and restore its normal function using regenerative medicine approaches, especially tissue engineering.
Research in tissue engineering and regenerative medicine encompasses all aspects of the research and development continuum from mechanistic studies to translational approaches.
Song Li, Ph.D., integrates principles of engineering, biomaterials and mechanobiology to advance cell and tissue engineering methods. He seeks to develop stem cell-based methods to promote regeneration in the heart and neuromuscular system and to advance immunoengineering approaches to treat cancer and other diseases.
His primary research area is to design and develop new biomaterial systems to provide fundamental bases and translational approaches to tissue engineering and regenerative medicine, particularly focusing on orthobiologics, material-based therapeutics to repair craniofacial and orthopedic skeletal defects, novel liposomal platform for drug and ...
Dr. Astgik Petrosyan‘s laboratory focuses on understanding the role of the extracellular matrix in cancer and development. She has expertise in tissue engineering, regenerative medicine, renal development, cancer, and chip technology.
Keywords: tissue engineering, regenerative medicine, perspective, directions Impact Statement This perspective article draws on the 7th TERMIS World Congress to showcase how innovations in tissue engineering and regenerative medicine are continuing to address global challenges. By exploring the interplay of science, ethics, and transla-
Oct 17, 2022 · The use of tissue engineering in regenerative medicine, known as TERM, is an active area of research that involves creating functional tissue through the combination of cells, scaffolds, and growth factors to restore normal biological function. 1 Clinicians treat millions of patients with tissue engineered regenerative devices. So far, the most ...
3 days ago · Tandon’s innovative research has focused on studying electrical signaling in the context of tissue engineering, and she has worked with cardiac, skin, bone, and neural tissue. This groundbreaking work in biomedical engineering has earned her recognition as one of Most Creative People in Business by Fast Company , an Innovation Fellow by WIRED ...
Three-Dimensional Bioprinting: A Comprehensive Review for Applications in Tissue Engineering and Regenerative Medicine Nicholas A. Mirsky, Quinn T. Ehlen, Jason A. Greenfield, Michael Antonietti, Blaire V. Slavin, Vasudev Vivekanand Nayak, Daniel Pelaez, David T. Tse, Lukasz Witek , Sylvia Daunert, Paulo Coelho
5 days ago · In the quest to advance regenerative medicine, the Harris Lab at Arizona State University is making groundbreaking strides. Focused on tissue regeneration and the intricate biology of cell death, the lab has uncovered a novel phenomenon with far-reaching implications for improving wound healing and injury repair. This research not only fills a critical gap in our understanding of necrotic ...
6 days ago · The PhD track in Tissue Engineering and Regenerative Medicine (TERM) prepares the students for a career in cutting edge research and development of cell- and biomaterial-based medical products.
Jan 9, 2025 · Irvine, Calif., Jan. 9, 2025 — An international research team led by the University of California, Irvine has discovered a new type of skeletal tissue that offers great potential for advancing regenerative medicine and tissue engineering.. Most cartilage relies on an external extracellular matrix for strength, but “lipocartilage,” which is found in the ears, nose and throat of mammals ...
Bladder tissue engineering and regeneration is an emerging field focused on developing innovative solutions for bladder repair and reconstruction, particularly in patients with bladder dysfunction ...