Works Cited
- Colten, Harvey R. “Extent and Health Consequences of Chronic Sleep Loss and Sleep Disorders—Sleep Disorders and Sleep Deprivation.” National Center for Biotechnology Information . U.S. National Library of Medicine, 01 Jan. 1970. Web. 03 Nov. 2016. .
- “Dangers of Getting Too Little Sleep.” HealthCommunities . N.p., n.d. Web. 03 Nov. 2016. .
- “Chronic Insomnia’s Dangerous Side-Effects.” Newsweek . Newsweek, 23 Aug. 2009. Web. 03 Nov. 2016. .
- “Chronic Insomnia Linked to Increased Risk of Death.” Mercola.com . N.p., n.d. Web. 03 Nov. 2016. .
Follow us on Reddit for more insights and updates.

Comments (0)
Welcome to A*Help comments!
We’re all about debate and discussion at A*Help.
We value the diverse opinions of users, so you may find points of view that you don’t agree with. And that’s cool. However, there are certain things we’re not OK with: attempts to manipulate our data in any way, for example, or the posting of discriminative, offensive, hateful, or disparaging material.
Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
More from Cause and Effect Essay Examples and Samples 2024

Jul 18 2023
How Your Childhood Affects Your Love Style Essay Sample Example
Apr 15 2019
How the Harry Potter Series Became So Popular Essay Sample, Example

Apr 05 2019
Why Our Ancestors Started to Walk on Two Feet Essay Sample, Example
Related writing guides, writing a cause and effect essay.
Remember Me
Is English your native language ? Yes No
What is your profession ? Student Teacher Writer Other
Forgotten Password?
Username or Email
Essay on Insomnia Disorder
A lack of sleep, or insufficient sleep, are symptoms of insomnia. Emotions, as well as bodies, are affected. Stress, sudden sadness, illness, and medication can induce sleeplessness. Hence, the best way to sleep is in a quiet environment. Insomnia is more common among the elderly. The Epworth Sleepiness Scale or a comparable test can detect insomnia. Emotional and physical symptoms may reflect concomitant disorders. Insomniacs may struggle to stay asleep, fall asleep, or wake up. There’s a lot to learn about autogenic, visualizing a look at the comorbidities of medicine and drug use (Blanken et al., 2019). Aided Devices Relax your body and mind with the Dream pad cushion. A weighted blanket designed for autistic people may help them sleep longer. Acute hypnotics should be used if nonpharmacological treatments fail. Exercise and massage are examples of complementary therapy. Chronic insomnia and daytime function improve after two years of CBT-I treatment. Personalized education reduces dropout rates. A new study shows that CBT helps with chronic insomnia. The digital CBT-I market is modest. More data on CBT’s components may lead to better therapy.
Introduction
The paper focuses on sleep-wake disorder and majorly on insomnia. Concerning this, one of the symptoms of insomnia is difficulty falling or staying asleep, or perhaps both. Insomnia is characterized by a lack of rest, reduced sleeping time, or complete sleep loss. Aside from making one feel weak and sleepy, it also hurts people’s emotions and capacity to operate for the rest of the day (Dauvilliers et al., 2020). If you have trouble falling asleep, often wake up throughout the night, or can’t go back to sleep at all, you may be suffering from poor quality sleep. This research, therefore, focuses on sleeplessness in more detail. Consequently, the report provides additional information about the disease, including assessing its severity and a battery of psychiatric tests. In this way, the article is educational since it will help folks who have sleep-wake issues.
Evaluation methods
Sleep medical and history, drug, and psychiatric histories determine if a patient has insomnia. Insomnia complaints, pre-sleep circumstances, sleep-wake cycles, other sleep-related symptoms, and daily effects should be included in the sleep history. For example, a patient’s medical, mental, or drug abuse history can be used to determine the kind and progression of insomnia and the variables that perpetuate it (Stein et al., 2018). Psychological screening tests, sleep diaries, symptom checklists, self-administered surveys, and bed partner interviews are all valuable tools in the examination and differential diagnosis of insomnia. Patients should look at the very least:
Co-occurring disorders can be identified using a questionnaire. Individuals and their accompanying problems can be identified using the Epworth Sleepiness Scale or another measure of drowsiness. A two-week sleep diary to track sleep-wake cycles and their day-to-day variations in general (Edinger et al., 2021a). Data from a sleep diary should be recorded before and during therapy and in the event of a relapse or a long-term reevaluation. Daytime function, quality of life, psychological assessment scales, and dysfunctional beliefs and attitudes can all be valuable tools in the initial assessment and outcome monitoring of patients with chronic insomnia. Comorbid disorders and possible diagnoses can be discovered by evaluating physical and mental states.
Patients with persistent insomnia should not be routinely evaluated using polysomnography or daytime multiple sleep latency testing (MSLT) since these tests are not appropriate for this purpose. Patients suspected of having respiratory or movement abnormalities (such as snoring) should have polysomnography done if the initial diagnosis is iffy, therapy fails (behavioral or pharmacological), or there are sudden awakenings with aggressive or aggressive, or harmful behaviors (Edinger et al., 2021a). People who have insomnia, significantly caused by depression, may benefit from the use of actigraphy to better understand their circadian rhythms and sleep disorders. In the absence of suspicion of concomitant diseases, no further tests are recommended to examine regularly examine chronic insomnia
Psychological Tests and Interviews
This part discusses Stimulus management, sleep compression, and relaxation training as interventions.
Stimulus control: Stimulation management is now a validated insomnia monotherapy. A stimulus can evoke several reactions based on past training. The bed and bedroom promote relaxation and sleep. Insomniacs have a history of participating in sleep-disrupting activities, including reading, eating, worrying, watching TV, and stimulating conversation. Oversleeping increases the probability of falling asleep, but excessive time in or near the bed decreases the possibility (Edinger et al., 2021a). When sleeping, the bed and bedroom might cause anxiety and stress. These states might be interoceptive markers for further arousal and sleep disruption. Discourage napping, use the bedroom for purposes other than sleep (or sex), and maintain regular bed and wake times. Nitrates are not advised for patients with mania, epilepsy, parasomnias, or in danger of falling
Sleep compression: Sleep compression treatment is an alternative to sleep restriction therapy. Treatments restricting how long a patient may stay in bed diminish their sleep time quickly, while those who slowly compress their time in bed do the opposite.
Relaxation: Relaxation techniques help many insomniacs. Hypervigilance or physical pain may impair adaptive sleep patterns in insomniacs. Relaxation approaches for treating insomnia include progressive muscle relaxation, autogenic training, visualization, and meditation. This approach’s tensing phase can be removed by passive progressive muscle relaxation (Stein et al., 2018). All relaxation methods require a calm, passive mindset and consistent relaxation to induce the parasympathetic response. The doctor encourages patient engagement in finding the most effective relaxing approach based on patient self-awareness. Finally, experience is crucial in eliciting the relaxation reaction. Relaxation training is a popular component of multicomponent insomnia treatments.
Medical Evaluation
Understanding chronic insomnia progression models help evaluate chronic insomnia from the perspectives of neurobiology, cognition, neurophysiology, behavior, and others. However, general model concepts are critical to identifying biopsychosocial predisposing factors, perpetuating factors, and precipitating factors. Illustrating the mental health-related behavioral and cognitive processes that perpetuate unpleasant thoughts and feelings may be incredibly beneficial (Dauvilliers et al., 2020). These procedures have remained primarily constant despite changes in models and diagnostic categories. In addition to complete patient history and examination, comorbidities such as medical, psychiatric, and medication/substance-related issues are considered.
Primary complaint
Insomniacs may have problems falling asleep, waking up frequently, staying asleep, having trouble returning to sleep, waking up too early in the morning, or not feeling refreshed, rested, or restorative throughout their sleep. Even though individuals may only report one symptom, it is normal for various symptoms to co-occur, and the precise presentation may change over time for different people (Blanken et al., 2019). First, it is essential to determine the complaint and how long it has been going on. Other factors to consider include how often it occurs (biweekly, weekly, or daily), how severe the symptoms are at night, how they manifest in the daytime, and how long it has been going on.
Pre-sleep conditions
Some insomnia patients establish habits that have the unintentional effect of continuing their sleep issues. Many of these habits may be traced back to attempts to “catch up” on sleep as a way to deal with sleep deprivation. Talking on the phone, using a computer, watching television, smoking, eating, exercising, or “clock watching” are all examples of activities that disrupt sleep (Edinger et al., 2021a). Patients with insomnia may be more aware of their surroundings than other people, and they may fear that they will have a stormy night’s sleep, which causes them to become more awake and nervous as the time for bed draws near. It’s helpful to know the patient’s emotional state and the sleeping environment while determining what influences sleep onset or sleep interruptions.
Relevant Ancillary Evaluations
This section will provide evaluation conducted by occupational therapists. As a result, it will discuss two evaluations.
Use of Assistive Devices: Relax your body and mind with the Dreampad pillow, a new patented technology that plays relaxing music as you sleep. The use of a weighted blanket, a sleep aid designed for people with autism spectrum disorders, may lengthen sleep cycles and minimize arousal times (Edinger et al., 2021b). The posture of preterm newborns has also been studied to see whether it might help them sleep better.
Use of activities: Two studies have looked at the effects of iRest meditation, yoga, and breathing exercises on helping people fall asleep. According to the studies analyzed, relaxing or contemplative activities can help people get a better night’s sleep, but the results aren’t consistent. Meditation was found to have a statistically more significant effect on sleep time than sleep hygiene instruction alone (Edinger et al., 2021a). Yoga and breathing methods were shown not to affect sleep duration, although they might help alleviate feelings of depression.
Evidence-Based treatment
Hypnotic medicines and nonpharmacological techniques, generally referred to as cognitive behavioral therapy for insomnia, are among the most effective therapies for insomnia (CBT-I). The CBT-I is made up of five primary parts, which include;
- What to do and what not to do when getting a good night’s sleep.
- Sleep deprivation: restricting the amount of time a person has to sleep to increase ‘proper’ night-time tiredness.
- Stimulus control: minimizing the amount of time spent awake in bed.
- Pre-sleep thoughts can be controlled by cognitive therapy.
- Physical methods of relaxing.
A wide range of non-specialist healthcare practitioners have shown to be successful in administering treatments (e.g., counselors, practice nurses, psychologists, health visitors). Improper hypnotic medication use has frequently been overlooked in favor of the more significant issue of insomnia treatment (Edinger et al., 2021a). As a result, these are the evidence-based approach to the treatment of insomnia.
Ensure that the insomnia criteria of chronicity and severity are met before beginning therapy. Comorbidity management is critical, but it may not alleviate the concomitant sleep issue. Sleep hygiene guidance is essential to the overall management plan (Edinger et al., 2021a). Evaluating one’s current way of life is necessary because the guidance addresses “problem” behaviors (excessive coffee use and irregular sleeping patterns). Strategies to prevent daytime sleepiness in acute care settings should also be investigated. Before prescribing hypnotic medicines, CBT-I for insomnia (including relaxation therapy) should be investigated. Patients should only be administered hypnotics for brief periods if they don’t react to nonpharmacological therapies or if nonpharmacological treatments are unavailable. Zaleplon, Zolpidem, Zopiclone, and the Short-Acting Benzodiazepines should be administered because there is no convincing evidence to discriminate between them.’ For hypnotic medicines, the recommended duration is four weeks maximum.
Evidence-based psychotherapies
Sleep restriction-sleep compression treatment and multicomponent cognitive-behavioral therapy have been acknowledged by Edinger et al., (2021a). A third treatment (stimulus control therapy) came close to meeting the requirements, but further research is needed to be sure (Dauvilliers et al., 2020). There isn’t enough data to recommend sleep hygiene, relaxation, or cognitive therapy instruction as stand-alone therapies for treating insomnia in older individuals at the moment. Thus they aren’t being considered. Other complementary therapies, including bright light therapy, massage, and exercise, should also be studied for their efficacy. According to this review, using the EBT coding manual’s recommended coding processes for assessing the current research on insomnia might lead to issues. More research is needed on the definition of older individuals as those aged 60 and above and the lack of a full assessment of medical comorbidities.

Psychiatric medication
Anticonvulsants.
Anticonvulsants like gabapentin and pregabalin can be used to treat insomnia. These drugs interfere with the wake-inducing effects of glutamate and norepinephrine (Edinger et al., 2021a). People who have primary insomnia have been found to benefit from using Tiagabine.
Antihypertensive
The antihypertensive medicine Prazosin (Minipress) has recently been shown to help patients who suffer from frequent nightmares and sleep disruption due to post-traumatic stress disorder. It is an antagonist of the adrenoreceptor. For the most part, individuals have been prescribed 2–6 mg, with a maximum dose of 15–20 mg based on the research done so far (Edinger et al., 2021a). A beginning dose of 1 mg is advised to avoid hypotension, gradually increasing until the desired therapeutic effect is obtained. The morning after a dosage increase is the most likely time for orthostatic hypotension. Thus, patients need to be warned about this risk. Military veterans and civilians with post-traumatic stress disorder (PTSD) treated with placebos found that prazosin helped them sleep better and reduced the number of nightmares they were experiencing.
Relevant ancillary treatment
Paradoxical intention.
Patients are taught to tackle their fear of staying awake and minimize the anxiety that goes along with it by accepting the condition of silent alertness until the onset of sleep using the paradoxical intention approach.
It consists of cognitive treatment, sleeps restriction therapy, stimulus control therapy, and relaxation therapy if desired. Even after two years of treatment with CBT-I, chronic insomnia and daytime function are markedly improved. It is the first-line treatment for older adults and those using hypnosis for a long time (Edinger et al., 2021b). It is possible to train the patient’s mind and body through autogenic and visualization to treat anxiety disorders. Even though the program requires many sessions, a two-session CBT-I program was more beneficial than generic sleep hygiene guidelines.
Relevant character strength
The effectiveness and efficiency of CBT-I (cognitive-behavioral treatment for insomnia) cannot be overstated. Digital CBT-I therapies that have been thoroughly established have been shown to lessen insomnia severity with effect sizes equivalent to face-to-face therapy. Dropout rates can be reduced by providing students with more individualized instruction. At least 18 months after starting Digital CBT-I, sleep metrics improved, and clinical insomnia severity was reduced (Edinger et al., 2021a). Anxiety and depression symptomatology improved even after 18 months, even though part of the posttreatment tiredness reductions was lost.
Digital CBT-I application and distribution are not well-understood in Edinger et al., (2021a) study. Even though scalability is a significant benefit, implementation and diffusion research methodologies have only been used in a few studies. A patient-centered approach to study design will be necessary to achieve this goal. Tens of millions of people worldwide will have easier access to treatment for insomnia because of digital CBT-I. Recent research findings did not include health care usage and quality-adjusted life years, which is unusual. Stand-alone digital CBT-I technologies have minor hurdles to entry into the industry.
For benzodiazepine and BZRA hypnotics, long-term efficacy is not a significant issue. Hypnotic drugs are helpful as a short-term therapy for insomnia. Because of this, doctors are left with little guidance when prescribing medications in specific sequences or combinations. When treating persistent insomnia, short-term pharmacological therapies alone are beneficial. Despite this, they fail to produce any lasting benefit even when stopped.
Individual medication vs. cognitive-behavioral treatment versus a combination of these techniques is more effective in treating chronic insomnia in the short run. Combined therapy studies have had conflicting outcomes. Combined therapy and cognitive-behavioral treatment do not seem to benefit from cognitive-behavioral treatment alone significantly.
There is a lack of data on the precise impacts of CBT’s many components, leading to more effective therapy and more precise customization. Even though meta-analyses show the benefit of CBT-I, they also point to substantial heterogeneity. When comparing results from different studies, it isn’t easy to pinpoint precisely which features of CBT-I were most responsible for the reported improvements in each one. As a result, research is required to provide this data.
Blanken, T. F., Benjamins, J. S., Borsboom, D., Vermunt, J. K., Paquola, C., Ramautar, J., Dekker, K., Stoffers, D., Wassing, R., & Wei, Y. (2019). Insomnia disorder subtypes are derived from life history and traits of effect and personality. The Lancet Psychiatry , 6 (2), 151–163.
Dauvilliers, Y., Zammit, G., Fietze, I., Mayleben, D., Seboek Kinter, D., Pain, S., & Hedner, J. (2020). Daridorexant, is a new dual orexin receptor antagonist to treat insomnia disorder. Annals of Neurology , 87 (3), 347–356.
Edinger, J. D., Arnedt, J. T., Bertisch, S. M., Carney, C. E., Harrington, J. J., Lichstein, K. L., Sateia, M. J., Troxel, W. M., Zhou, E. S., & Kazmi, U. (2021a). Behavioral and psychological treatments for chronic insomnia disorder in adults: An American Academy of Sleep Medicine clinical practice guideline. Journal of Clinical Sleep Medicine , 17 (2), 255–262.
Edinger, J. D., Arnedt, J. T., Bertisch, S. M., Carney, C. E., Harrington, J. J., Lichstein, K. L., Sateia, M. J., Troxel, W. M., Zhou, E. S., & Kazmi, U. (2021b). Behavioral and psychological treatments for chronic insomnia disorder in adults: An American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. Journal of Clinical Sleep Medicine , 17 (2), 263–298.
Stein, M. B., McCarthy, M. J., Chen, C.-Y., Jain, S., Gelernter, J., He, F., Heeringa, S. G., Kessler, R. C., Nock, M. K., & Ripke, S. (2018). Genome-wide analysis of insomnia disorder. Molecular Psychiatry , 23 (11), 2238–2250.
Cite This Work
To export a reference to this article please select a referencing style below:
Related Essays
China’s electric vehicle (ev) market, mental disorders: schizophrenia, nursing assignment: evaluating health information, adult clinical discussion, seabird-habitat association of the merginae family research study, open-ended question essay on pain modulation, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail
Insomnia: Cause and Effect Essay
Insomnia is a prevalent mental disorder affecting a significant portion of the population. It manifests as a difficulty in sleeping and can become chronic after a certain period. Despite its prominence, the mechanisms behind insomnia’s causes are still not fully explored. The same applies to the disorder’s potential outcomes, the research into which is ongoing. However, some facts are well-established, which allows healthcare specialists to treat insomniac patients and predict/prevent the associated diseases. The essay will highlight what is known about insomnia’s epidemiology and its effects as far as a person’s health is concerned, although it also affects other aspects of one’s life.
Insomnia can have many precursors, some of which will lead to other conditions. For instance, the hypothalamic-pituitary-adrenal axis is said to cause the disorder if it experiences dysregulations (Javeheri & Redline, 2017). The consequences include the elevated activity of the sympathetic nervous system and hormonal imbalance (Javeheri & Redline, 2017). As a result, a person begins experiencing insomnia, which can manifest as a short sleep duration (Javeheri & Redline, 2017). The latter is directly associated with such cardiovascular conditions as hypertension, heart failure (HF), and coronary heart disease (Javeheri & Redline, 2017). They are mostly responsible for mortality cases in insomniac patients as the disorder itself is not lethal, but its consequences may endanger one’s life (Javeheri & Redline, 2017). On the other hand, HF is one of insomnia’s causes, which creates a cycle when one cardiovascular disease leads to insomnia, and it subsequently increases the incidence risk of similar outcomes (Javeheri & Redline, 2017). Thus, insomnia is a result of the dysregulated hypothalamic-pituitary-adrenal axis and, in turn, induces heart conditions with severe effects on one’s well-being, although a cardiovascular disease may also trigger insomnia.
Another prominent cause of insomnia is rooted in genetics, which has been established through family and twin studies. They indicate that the disorder is inheritable to a moderate degree, while the female population is more likely to be affected (Lind & Gehrman, 2016). Although examining twins contributed significantly to proving insomnia’s heritability, determining the exact genes responsible for its development remains challenging due to phenotype inconsistencies (Lind & Gehrman, 2016). Both serotonin and dopamine transporters are subject to genetic studies, and their association with insomnia continues to be supplied with more evidence (Lind & Gehrman, 2016). Their role is to cause hyperarousal through wake-promoting neurons, which prompts insomnia (Lind & Gehrman, 2016). The disorder’s inheritable nature is also evident due to its occurrence in children, who are less susceptible to other common stressors (Lind & Gehrman, 2016). Genetically, insomnia tends to be linked with similar mental conditions but may also result in such a physical health outcome as diabetes because a correlation exists between it and sleep duration (Lind & Gehrman, 2016). Overall, insomnia can be a genetic condition and entail type 2 diabetes, although the connection requires further studies.
Insomnia manifests as a response to trauma, which makes it related to other mental disorders. The traumatizing experience may occur in one’s childhood or adulthood: they differ in rapid eye movement fragmentation, with the former causing its increased form (Hertenstein et al., 2018). As a result, people develop certain conditions, varying from insomnia to depression, and their occurrence depends on many factors (Hertenstein et al., 2018). For instance, an insomniac person is unlikely to have post-traumatic stress disorder beforehand; moreover, such a trait as sleep reactivity makes one more susceptible to insomnia than other outcomes (Hertenstein et al., 2018). Whether the traumatic event happened as a result of the patient’s actions or beyond their control also matters: the former is more likely to provoke guilt and shame, which increases insomnia’s likelihood (Hertenstein et al., 2018). However, even if comorbidity does not develop initially, the latter will still serve as a foundation for other mental disorders (Hertenstein et al., 2018). Insomnia increases the risk of anxiety, depression, psychosis, and alcohol abuse, with the first two being particularly prominent outcomes (Hertenstein et al., 2018). Altogether, insomnia may be caused by trauma and induce other mental conditions.
Insomnia has multiple causes, and its health outcomes are also varied. One of the phenomena triggering it is the dysregulated hypothalamic-pituitary-adrenal axis, which affects the nervous system and hormones. As a consequence, insomnia develops and leads to cardiovascular conditions, which may significantly threaten a person’s well-being. Another cause is genetics, meaning that the disorder is inheritable by some of the population, affecting dopamine and serotonin transporters responsible for hyperarousal. In that case, insomnia may result in type 2 diabetes, which also has genetic correlations. Lastly, insomnia occurs as a trauma response, substituting other disorders, such as anxiety and PTSD, but it does not completely negate them. Furthermore, they tend to develop later due to sleep shortness, which is one of insomnia’s symptoms. Judging by the studied information, insomnia presents a vicious cycle, being both an outcome of another disorder or its main cause, insinuating that an afflicted person may struggle with treating the condition.
Hertenstein, E., Feige, B., Gmeiner, T., Kienzler, C., Spiegelhalder, K., Johann, A., Jansson-Fröjmark, M., Palagini, L., Rücker, G., Riemann, D., & Baglioni, C. (2018). Insomnia as a predictor of mental disorders: A systematic review and meta-analysis . Sleep Medicine Reviews, 43 , 96-105.
Javaheri, S., & Redline, S. (2017). Insomnia and risk of cardiovascular disease . Chest, 152 (2), 435-444.
Lind, M., & Gehrman, P. (2016). Genetic pathways to insomnia . Brain Sciences, 6 (4), 64-81.
- Traumatic Brain Injury: The Functional Independence Measure and the Patient Treatment
- Polycystic Ovary Syndrome: Medication Management
- Emotional and Anxiety Disorders and Social Cognition
- AUD: Psychopharmacologic Treatments
- The Definitions of Insomnia
- Research on Five Common Conditions
- Statistics for Health Care Research: The T-Values
- Chronic Hepatitis B in Chicago Area Analysis
- Hypergranulation Tissue: Causes and Treatment
- Effective Facial Moisturizers for Skin
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, July 7). Insomnia: Cause and Effect. https://ivypanda.com/essays/insomnia-cause-and-effect/
"Insomnia: Cause and Effect." IvyPanda , 7 July 2022, ivypanda.com/essays/insomnia-cause-and-effect/.
IvyPanda . (2022) 'Insomnia: Cause and Effect'. 7 July.
IvyPanda . 2022. "Insomnia: Cause and Effect." July 7, 2022. https://ivypanda.com/essays/insomnia-cause-and-effect/.
1. IvyPanda . "Insomnia: Cause and Effect." July 7, 2022. https://ivypanda.com/essays/insomnia-cause-and-effect/.
Bibliography
IvyPanda . "Insomnia: Cause and Effect." July 7, 2022. https://ivypanda.com/essays/insomnia-cause-and-effect/.
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
- Insomnia: Causes, Symptoms, and Treatment Words: 797
- Insomnia and Its Negative Health Effects Words: 1151
- Insomnia and Sleep Disorders Words: 643
- Insomnia in a Young Man: Possible Reasons and Treatment Words: 669
- Insomnia and Sleep Disorders Analysis Words: 698
- Depression: Symptoms, Causes and Treatment Words: 947
- Insomnia and Sleep Disorders Prevention and Management Words: 612
- Scoliosis: Causes, Effects, Prevention and Treatment Words: 1289
- Diabetes: Causes, Treatment, and Magnitude Words: 2345
- Developing Patient Treatment Plan Words: 943
- Depression in Adolescence: Causes and Treatment Words: 805
- Atherosclerosis: Pathophysiology, Treatment and Patient Education Words: 2791
- Rheumatoid Arthritis: Causes and Treatment Words: 1557
- Amyotrophic Lateral Sclerosis: Causes, Symptoms, and Treatments Words: 2511
- The Effects of Seclusion on Mentally Ill Patients Words: 1755
- Anorexia Nervosa: Causes, Symptoms, and Treatment Words: 1221
- Child Abuse: Risks, Causes, Effects, Treatment Words: 2037
Insomnia: Causes and Treatment
This study aimed to explore to root causes of sleep disturbances, sleeping pills use, and their subsequent side effects among insomniacs. Insomnia is a common health challenge globally with severe health challenges. A thematic analysis was conducted on data obtained from the messageboard posts by seven patients. The findings indicated that there were different causes of insomnia, different methods of interventions and side effects of prescribed sleeping pills. Patients displayed different symptoms, treatment outcomes and adverse effects of drugs. It was concluded that insomnia is a serious medical condition that required individualised intervention or a combination of interventions to avoid certain side effects of self-administered sleeping pills.
Introduction
Sleep disturbances and their related consequences are common among adults and a part of human experiences, as many studies have indicated (Dyas et al., 2010; Moloney, Konrad, & Zimmer, 2011). Insomnia affects many people globally. For instance, over one-third of adults in the UK and North America have reported insomnia (Dyas et al., 2010). Women are more susceptible to sleep disturbances relative to their male counterparts, and the condition increases with age (Morlock, Tan, & Mitchell, 2006). Insomnia has costly consequences such as dysfunction, perturbed diurnal waking state, absenteeism from work, poor quality of life and dependence on sleeping pills.
More than one-third of people with sleep disturbances experience recurring symptoms or chronic conditions. In most cases, insomnia is comorbid and has been associated with physical abuse, depression, anxiety, chronic pain and other physical challenges. Evaluation of patients’ condition is imperative, but effective treatment of the condition leads to better outcomes and improved quality of life.
As studies have shown, most people with insomnia seek medical attention from general practitioners first (Touitou, 2007). Services provided may differ from one GP to another. Patients must confront a new diagnosis, which could be frightening, and doctors often offer sleep hygiene education and prescriptions. Reported cases of insomnia have demonstrated that there is a need to enhance the management of sleep challenges through effective medications, patient education, evidence-based practices noted in psychosocial interventions such as cognitive behavioural therapy.
To offer effective management and enhance patients’ experiences of care for insomnia, it is imperative to understand patients’ beliefs and conditions of the problem and their expectations. In most cases, however, general practitioners have often offered sleeping pills to manage cases of chronic insomnia. Like any other drugs, these drugs have different side effects on different patients. Most users have reported daytime drowsiness and confusion at night. Sleeping pills are powerful hypnotics and could be helpful, but sleep may persist after patients have woken up. Pagel (2005) had observed that previous sleeping pills used to induce sleep were dangerous and addictive, and clinicians failed to address the major causes of the problem. Over the years, however, sleep medications have improved, and understanding sleep problems have increased significantly. It is imperative to take sleeping pills at the right time to avoid daytime side effects. Drugs such as Ambien and Lunesta are common, and patients use them before going to bed. Sleeping pills are effective when taken at the right time, i.e., when one can get a full night of sleep, between seven to eight hours before waking up. A recent study has demonstrated that patients take their sleeping pills in the middle of the night (Roth et al., 2013). These are mainly associated with self-medication tendencies among insomniacs. It is a source of concern as patients become prone to self-administered drugs after nocturnal awakenings, yet little efficacy or safety data exist to support such usages.
This thematic analysis aimed to explore root causes of sleep disturbances, sleeping pills use and other interventions and their subsequent side effects among insomniacs. The study would form part of themes that define causes, pills interventions, and their side effects and outcomes in attempts to manage sleep challenges.
Do clinicians apply integrative approaches or interventions to treat insomnia in patients?
To answer this question, the study had to explore the causes of insomnia, interventions and outcomes of treatments provided.
This topic is important for understanding insomnia, its causes, interventions and outcomes, and therefore, it would contribute to treatment and management.
A qualitative study was conducted using online message board posts for patients with insomnia to explore root causes of sleep disturbances, sleeping pills use, and their subsequent side effects. The researcher was interested in patients’ experiences with different drugs and side effects so that the study could provide majors themes in sleep disturbances management.
A thematic analysis was used to identify major themes in the message board posts. The researcher believed that thematic analysis would provide an accessible and theoretically flexible approach to analyse qualitative data (Braun & Clarke, 2006).
Participants
Participants for the study were chosen from the messageboard posts. They consisted of male and female patients who had suffered insomnia for several years. There were seven participants, consisting of four male and three female chosen randomly from the messageboard. Participants were aged between 26 and 85 years old. These participants were Americans and British. Participants were a good sample because they could offer thematic concerns for sleeping pills use among people with sleeping disturbances. Moreover, they originated from different continents to reflect if treatments and experiences were similar.
Texts for the study were obtained from https://www.everydayhealth.com/ . These posts were made between the year 2010 and 2011. Revolution health was health-based Web site and accessible to global users. Everyday Health provides materials for health education purposes on different health issues to different visitors. It also discusses current health issues to provide personalised health programmes for everyday living (Everyday Health, Inc., 2014).
Data from this Web site were appropriate for the study because of wide coverage and diverse contributions from users or patients.
Procedure and ethics
Data were obtained from the website, as mentioned above. Participants were randomly selected based on their posts, age and gender regarding insomnia. Only relevant texts to the study themes were selected for analysis. Texts were left in their original forms to capture true comments or themes.
Texts were analysed based on themes. Posts were reviewed and coded to identify similar themes. This process was repeated several times to refine and capture three major themes and their sub-themes. Although patients provided different accounts of their experiences, only relevant themes were selected for the study.
Although all study participants provided their names and locations, no names were captured in the analysis. Instead, anonymity was maintained during the coding process by using P1, P2 to P7 for all patients in the study. The material used was readily available from the public domain.
There was no ethical approval for this study because no human subject was directly involved.
This thematic analysis aimed to explore root causes of sleep disturbances, sleeping pills use and their subsequent side effects among insomniacs.
One can simply identify themes as causes, interventions and outcomes or side effects of treatment. Critically, the study showed that there is no single cause of insomnia; sleeping pills alone were common for intervention, but were not effective and had severe side effects. That is, general practitioners did not address the root causes of insomnia.
To answer the research question, the study showed that general practitioners did not use integrative interventions to treat insomnia, but rather prescribed sleeping pills alone, which could not address the root causes of the problem.
Table 1: Table of themes on causes, interventions, and side effects of sleeping pills
Patients with insomnia described different causes of their conditions. For instance, causes of insomnia were related to past physical abuse, lack of care, certain diseases, worrying, anxiety, depression, certain life crisis and tinnitus, among others. These sub-themes showed that causes of insomnia varied among different persons, between male and female and patient of different ages. For instance, P7 wrote that his insomnia resulted from tinnitus .
Patients also used different means to manage insomnia. Majorities sought help from general practitioners, who prescribed sleeping pills. Other patients used different methods, including physical exercise and yoga. It is imperative to note that pills were self-administered, and patients could easily change them, use them at different periods or combine them when they wish. For instance, P6 used a combination of pills and later noted thus, “ I decided to try my experiment – I would take a 30-day supply of Lunesta, followed by a 30-day supply of Ambien, testing to see which was more effective for me ”.
Although some patients reported a lack of side effects with certain pills, majorities reported cases of pain, effects on physical and mental health associated with fatigue, dizziness, anxiety and depression and causes of abnormal behaviours.
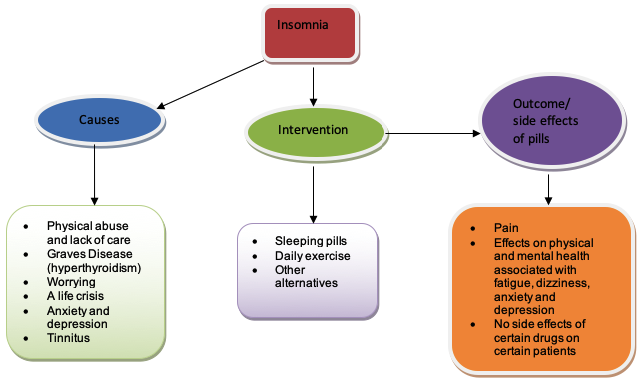
Note: ovals show major themes, boxes show sub-themes and arrows show relationships
Three major themes were noted after thematic analysis of the posts on insomnia. Patients mentioned causes, interventions and side effects. Causes of insomnia varied from patient to patient. Still, generally, a history of physical abuse, life crisis, depression, anxiety, use of certain medications and tinnitus were responsible for insomnia among patients who took part in the study. Moloney et al. (2011) noted that ‘medicalization’ was contributing to insomnia in the US. The condition affected patients of both sexes with different ages (Morlock et al., 2006). Severity and effects of insomnia differed among patients.
Generally, many patients consulted their general practitioners when their conditions persisted. Previous studies by Dyas et al. (2010) had shown similar outcomes. Many clinicians did not address the root causes of insomnia. In this study, patients showed that they only received prescribed sleeping pills from general practitioners while there were no attempts to address the root causes of insomnia. Except for the patient who combined medication and exercise and reported positive improvements, others reported continued pain, abnormal behaviours, fatigue and dizziness among other side effects. Other studies have shown that sleeping pills had such side effects, particularly when self-administered (Roth et al., 2013). Patients had tendencies to self-administer sleeping pills, a practice that exposed them to adverse effects of such pills (Roth et al., 2013). It is therefore imperative to use sleeping pills alongside other interventions, such cognitive behavioural therapy to address root causes of insomnia.
Sleeping pills exposed patients to different forms of side effects. However, not all patients experienced similar side effects, while others did not experience such side effects at all with certain pills. This indicates that insomnia resulted from different causes, therefore, required different approaches. No specific interventions were appropriate for all patients. Therefore, clinicians need to understand the side effects of sleeping pills on their patients. Patients must also understand that self-administration of different drugs caused adverse effects on their health.
While this study provided significant insights on thematic issues in insomnia, it had some limitations. Data were gathered from patients’ posts, which did not capture certain data. Moreover, patients did not follow any guideline in their responses and issues of bias were not controlled. A small sample was also used in this study. Nevertheless, the study highlighted failures by patients to adhere to prescription and a lack of patient education on their conditions.
The study implications focus on clinicians and their roles. There is a need to educate patients on the risks of self-administered sleeping pills. Moreover, clinicians should understand the root causes of insomnia before prescribing sleeping pills because pills do not address causes of sleep disturbances.
In conclusion, insomnia is a serious medical condition that requires individualised intervention or a combination of interventions, including cognitive behavioural therapy, to avoid certain side effects from self-administered sleeping pills.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77-101.
Dyas, J., Apekey, T., Tilling, M., Ørner, R., Middleton, H., & Siriwardena, N. (2010). Patients’ and clinicians’ experiences of consultations in primary care for sleep problems and insomnia: a focus group study. British Journal of General Practice, 60(574), e180–e200. Web.
Everyday Health, Inc. (2014). Company Overview. Web.
Moloney, M., Konrad, T., & Zimmer, C. (2011). The Medicalization of Sleeplessness: A Public Health Concern. American Journal of Public Health, 101(8), 1429–1433. Web.
Morlock, R., Tan, M., & Mitchell, D. (2006). Patient characteristics and patterns of drug use for sleep complaints in the United States: analysis of National Ambulatory Medical Survey data, 1997-2002. Clinical Therapeutics, 28(7), 1044-53.
Pagel, J. (2005). Medications and their effects on sleep. Primary Care, 32(2), 491-509.
Roth, T., Berglund, P., Shahly, V., Shillington, A., Stephenson, J., & Kessler, R. (2013). Middle-of-the-Night Hypnotic Use in a Large National Health Plan. Journal of Clinical Sleep Medicine, 9(7), 661-668. Web.
Touitou, Y. (2007). Sleep disorders and hypnotic agents: medical, social and economical impact. Annales Pharmaceutiques Françaises, 65(4), 230-8.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2020, September 18). Insomnia: Causes and Treatment. https://studycorgi.com/insomnia-causes-and-treatment/
"Insomnia: Causes and Treatment." StudyCorgi , 18 Sept. 2020, studycorgi.com/insomnia-causes-and-treatment/.
StudyCorgi . (2020) 'Insomnia: Causes and Treatment'. 18 September.
1. StudyCorgi . "Insomnia: Causes and Treatment." September 18, 2020. https://studycorgi.com/insomnia-causes-and-treatment/.
Bibliography
StudyCorgi . "Insomnia: Causes and Treatment." September 18, 2020. https://studycorgi.com/insomnia-causes-and-treatment/.
StudyCorgi . 2020. "Insomnia: Causes and Treatment." September 18, 2020. https://studycorgi.com/insomnia-causes-and-treatment/.
This paper, “Insomnia: Causes and Treatment”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: September 18, 2020 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
Home — Essay Samples — Nursing & Health — Insomnia — Insomnia: It’s Causes, Symptoms and Effects
Insomnia: It's Causes, Symptoms and Effects
- Categories: Insomnia
About this sample

Words: 964 |
Published: Dec 18, 2018
Words: 964 | Pages: 2 | 5 min read
Table of contents
Causes of insomnia, chronic insomnia, symptoms of insomnia.
- Insomnia can be caused by unhealthy sleep habits, specific substances, psychiatric and medical conditions, and/or certain biological factors. Recently, researchers have begun to think about insomnia as a problem of your brain being unable to stop being awake because our brain has a sleep cycle and a wake cycle (when one is turned on the other is turned off). Insomnia can be a problem with either part of this cycle; it can be too much wake drive or too little sleep drive. It’s important to first understand what could be causing your sleep difficulties.
- Mental health disorders: Anxiety disorders, such as post-traumatic stress disorder, may disrupt your sleep. Awakening too early can be a sign of depression. Insomnia often occurs with other mental health disorders as well.
- Medications: Many prescription drugs can interfere with sleep, such as certain antidepressants and medications for asthma or blood pressure. Many over-the-counter medications such as some pain medications, allergy and cold medications, and weight-loss products contain caffeine and other stimulants that can disrupt sleep.
- Medical conditions: Conditions linked with insomnia include chronic pain, cancer, diabetes, heart disease, asthma, gastro esophageal reflux disease (GERD), overactive thyroid, Parkinson’s disease and Alzheimer’s disease.
- Sleep-related disorders: Sleep apnea causes you to stop breathing periodically throughout the night, interrupting your sleep. Restless legs syndrome causes unpleasant sensations in your legs and an almost irresistible desire to move them, which may prevent you from falling asleep.
- Caffeine, nicotine and alcohol: Coffee, tea, cola and other caffeinated drinks are stimulants. Drinking them in the late afternoon or evening can keep you from falling asleep at night. Nicotine in tobacco products is another stimulant that can interfere with sleep. Alcohol may help you fall asleep, but it prevents deeper stages of sleep and often causes awakening in the middle of the night.
- Changes in sleep patterns: Sleep often becomes less restful as you age, so noise or other changes in your environment are more likely to wake you. With age, your internal clock often advances, so you get tired earlier in the evening and wake up earlier in the morning. But older people generally still need the same amount of sleep as younger people do.
- Changes in activity: You may be less physically or socially active. A lack of activity can interfere with a good night’s sleep. Also, the less active you are, the more likely you may be to take a daily nap, which can interfere with sleep at night.
- Changes in health: Chronic pain from conditions such as arthritis or back problems as well as depression or anxiety can interfere with sleep. Issues that increase the need to urinate during the night such as prostate or bladder problems can disrupt sleep. Sleep apnea and restless legs syndrome become more common with age.
- Stress: Concerns about work, school, health, finances or family can keep your mind active at night, making it difficult to sleep. Stressful life events or trauma — such as the death or illness of a loved one, divorce, or a job loss — also may lead to insomnia.
- Travel or work schedule. Your circadian rhythms act as an internal clock, guiding such things as your sleep-wake cycle, metabolism and body temperature. Disrupting your body’s circadian rhythms can lead to insomnia. Causes include jet lag from traveling across multiple time zones, working a late or early shift, or frequently changing shifts.
- Poor sleep habits. Poor sleep habits include an irregular bedtime schedule, naps, stimulating activities before bed, an uncomfortable sleep environment, and using your bed for work, eating or watching TV. Computers, TVs, video games, smartphones or other screens just before bed can interfere with your sleep cycle.
- Eating too much late in the evening. Having a light snack before bedtime is OK, but eating too much may cause you to feel physically uncomfortable while lying down. Many people also experience heartburn, a backflow of acid and food from the stomach into the esophagus after eating, which may keep you awake.
- Difficulty falling asleep at night.
- Waking during the night.
- Waking earlier than desired.
- Still feeling tired after a night’s sleep.
- Daytime fatigue or sleepiness.
- Irritability, depression, or anxiety.
- Poor concentration and focus.
- Being uncoordinated, an increase in errors or accidents.
- Tension headaches (feels like a tight band around head).
- Difficulty socializing.
- Gastrointestinal symptoms.
- Worrying about sleeping.

Cite this Essay
To export a reference to this article please select a referencing style below:
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof. Kifaru
Verified writer
- Expert in: Nursing & Health
+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
4 pages / 1922 words
2 pages / 790 words
2 pages / 979 words
1 pages / 547 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Did you know that milk collected at night might actually help with anxiety and insomnia? Sounds a little odd, right? However, according to research published in the Journal of Medicinal Food earlier this year, it could be [...]
The aim of the research that was done in this paper is to find out if there is any two-direction connection between anxiousness (anxiety) and helplessness (depression) on one side while sleeplessness (insomnia) on the other side [...]
Dyssomnias are characterized by the amount, quality and/or timing of sleep. The five specific types of dyssomnias are: primary insomnia, primary hypersomnia, narcolepsy, breathing-related sleep disorder, and circadian rhythm [...]
“The Yellow Wallpaper” by Charlotte Perkins Gilman tells the story of a young woman who was taken by her husband to a new home because he had diagnosed her with being just a tad hysterical. Gilman wrote this poem shortly after a [...]
People throughout the world tend to struggle with different issues that hold them back in some way or another. Some issues can affect a person’s health and lead to drastic changes in a person’s brain. In order for a person to [...]
Biological factors regarding pathological gambling have been studied by Illinois Institute for Addiction Recovery which implied that chemical addiction and gambling addiction are similar. It has been found that pathological [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

IMAGES
COMMENTS
Nov 4, 2016 · One of the most common health problems of modernity is insomnia—or, how it is also often called, sleep deprivation. Its prevalence is caused by the fact that it, firstly, accompanies a large number of mental conditions (starting from regular anxiety and/or frustration, and ending up with depression, obsessive-compulsive disorder, and so on), and secondly, by a number of environmental factors ...
Jun 13, 2024 · The economic impact of insomnia is also significant, with increased healthcare costs, absenteeism, and reduced work efficiency contributing to substantial financial burdens on both individuals and society. Addressing the mental health and productivity consequences of insomnia is essential for fostering a healthier, more productive population.
Introduction. The paper focuses on sleep-wake disorder and majorly on insomnia. Concerning this, one of the symptoms of insomnia is difficulty falling or staying asleep, or perhaps both. Insomnia is characterized by a lack of rest, reduced sleeping time, or complete sleep loss.
Apr 12, 2024 · Insomnia can be diagnosed and treated using multiple ways. Medical professionals often diagnose insomnia through a combination of a physical exam, a sleep habit review, and a sleep study. Once diagnosed, insomnia is treated by addressing the underlying causes and their symptoms, including stress (NHS, 2022).
Writing an essay about insomnia is an important way to raise awareness and provide helpful information to those who are struggling with sleep. Whether you choose to write an argumentative, cause and effect, opinion, or informative essay, there are plenty of topics to explore and examples to draw inspiration from.
Symptoms to look out for if you think you have insomnia. Now that you already know a little bit more about insomnia itself, it’s time to talk about the symptoms. You have trouble sleeping. You think that you have some sort of listed above problems. Now you are wondering do you suffer from insomnia.
Jul 7, 2022 · Insomnia increases the risk of anxiety, depression, psychosis, and alcohol abuse, with the first two being particularly prominent outcomes (Hertenstein et al., 2018). Altogether, insomnia may be caused by trauma and induce other mental conditions. Insomnia has multiple causes, and its health outcomes are also varied.
Sep 18, 2020 · Patients displayed different symptoms, treatment outcomes and adverse effects of drugs. It was concluded that insomnia is a serious medical condition that required individualised intervention or a combination of interventions to avoid certain side effects of self-administered sleeping pills. Introduction
Dec 18, 2018 · Symptoms of Insomnia. Insomnia itself may be a symptom of an underlying medical condition. However, there are many signs and symptoms that are associated with insomnia: Difficulty falling asleep at night. Waking during the night. Waking earlier than desired. Still feeling tired after a night’s sleep. Daytime fatigue or sleepiness.
Paper Type: 650 Word Essay Examples Cause And Effect Essay Sleeplessness, commonly referred to as insomnia, has become a widely discussed topic in today's increasingly complex world. Extensive research has been conducted to uncover the underlying causes and the far-reaching effects of this condition.