- E-mail: [email protected]

- IELTS Practice Tests
- Recent Actual Tests
- Speaking Part 1
- Speaking Part 2
- Speaking Part 3
- General Training Writing Task 1
- Process Diagram
- Mixed Charts
- Advantages & Disadvantages Essays
- Agree or Disagree Essays
- Discuss Both Views Essays
- Direct Questions Essays
- Problems/Causes & Solutions Essays
- Speaking Vocabulary
- Writing Vocabulary
- Collocations for IELTS

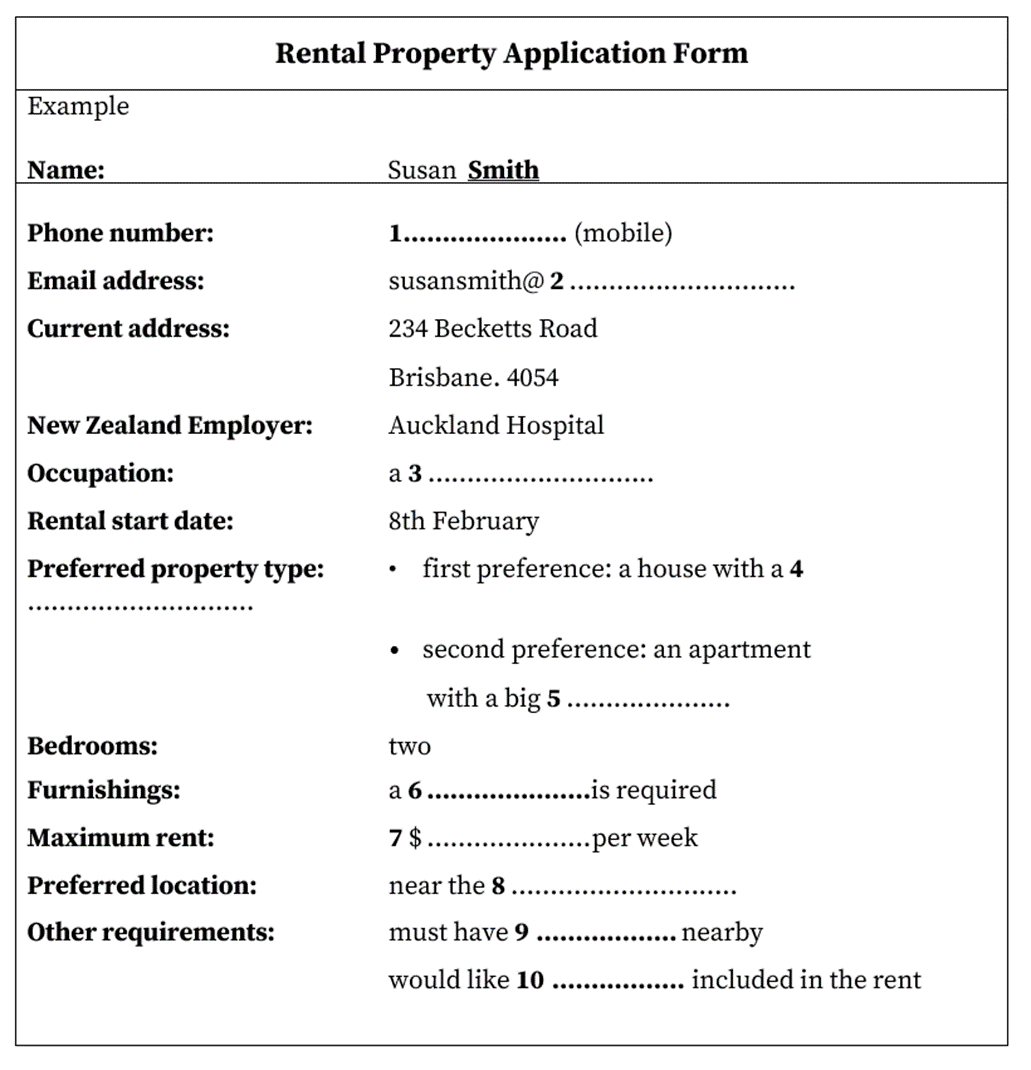
IELTS Listening Practice Test 204

Questions 1-10
Complete the form below
Write ONE WORD AND/OR A NUMBER for each answer.
Questions 11-20
Complete the notes below.
Write NO MORE THAN THREE WORDS AND/OR A NUMBER for each answer.
The Pre-school Family Centre
Features of the Pre-school Family Centre
- for children from 11……………… to 5 years old
- run as a 12……………….. by parents, who attend with their children
- parents receive special 13……………… from the centre
- children’s activities organised in 14 ……………. age groups
Facts about the Centre
- sessions from 9.30 − 12.30 each morning
- one afternoon session to help prepare older children for 15 at school
- parents must make several 16 ……………… before they enrol their child
- each centre is officially recognised and receives 17 …………………. funding
Parents’ Commitments
- take on responsibility for a special 18 ……………………..
- attend one 19 ……………………..
Practical Advice
- attend regularly to help your child gain 20 ……………………..
- younger children may need to leave early
- provide a snack for your child
Questions 21-30
Questions 21−26
Choose the correct letter, A, B or C.
Presentation on foot injuries among sports players
21. John and Cath’s presentation plans are different in
A. the examples used.
B. the order of information.
C. the main points made.
22. What do the students agree about the anatomy section of their presentation?
A. It would be better if Cath spoke about it.
B. It should be kept quite short.
C. It should be based on information from the internet.
23. What do the students agree to include in the last section?
A. visuals of injuries
B. demonstrations of treatment
C. interviews with patients
24. What is said about the different types of heel injury?
A. Diagnosis is straightforward.
B. They are expensive to treat.
C. Some are more serious than others.
25. On the subject of causes of heel injuries, the students agree to
A. focus on a single reason.
B. reject certain approaches.
C. use a source written by their professor.
26. What does Cath say about stretching as a treatment?
A. It is potentially risky.
B. It is commonly confused with strengthening,
C. It is the least effective part of treatment.
Questions 27 and 28. Choose TWO letters A-E .
Which TWO treatment techniques did the female runner find useful for her swollen heel?
A massage
B ultrasound
C rest
D balancing exercises
E ice
Questions 29 and 30. Choose TWO letters, A-E .
Which TWO sports did the male sprinter find most effective during his rehabilitation programme?
A swimming
B weight−training
C running on grass
D cycling
E jumping
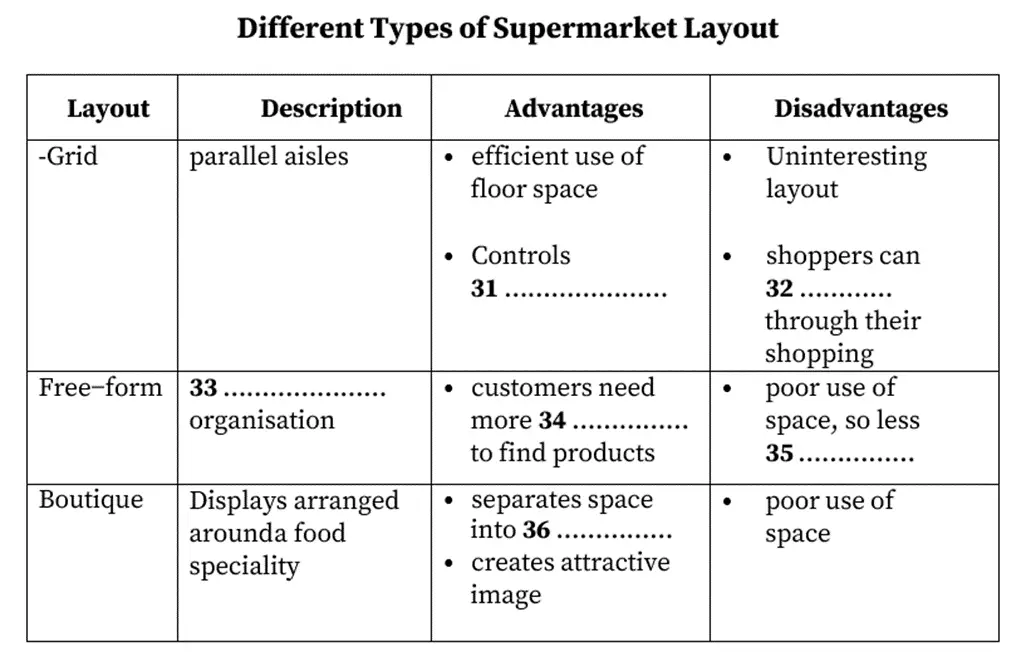
Questions 31-40
Questions 31−36 Complete the table below.
Write NO MORE THAN THREE WORDS for each answer.
1. 614381997
2. post.com
10. electricity
11. 3 months
12. cooperative
13. training
15. reading
17. government
19. meeting
20. confidence
31. traffic flow
35. const-effective
36. smaller areas
Pros & Cons of Computer Delivered IELTS: Experts’ Views
Some people like to try new things, for example, places to visit.
1- 614381997 2- post.com 3- cecet 4-own garden 5- balcony 6- fredige 7- 350 8- bridge 9- parking 10- electricty bill 11- 3 months 12- occuoacy 13- training 14-mixed 15- reading 16- visits 17- official 18- job 19- meeting 20- confident 21- A 22- B 23- B 24- C 25- A 26- A 27- rest 28- massage 29- cycling 30- weight training 31-traffic flow 32- rush 33- random patren 34- time 35- space 36- small area
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
POPULAR POSTS
Cambridge ielts 1-19 book series [pdf + audio], cambridge ielts 19 academic [pdf + audio], cambridge ielts 18 academic [pdf + audio], 200 ielts speaking sample answers [pdf + audio], ielts recent actual tests [full pdf + audio], cambridge ielts 18 general training [pdf + audio], cambridge ielts 17 general training [pdf + audio], cambridge ielts 17 academic [pdf + audio], ielts reading practice test 320.

9IELTS is dedicated to providing free materials and resources for IELTS conquerors. Stay constantly updated with a wide range of ultimate tips, strategies, and practice tests to crack the high-stakes IELTS exam!
Recent Posts
Ielts reading practice test 185, describe a typical day when you are not working or studying, ielts reading practice test 277, what sort of punishment should be allowed to use to teach children, describe a time when you had to change your plan.
- Terms & Conditions
- Privacy Policy
© 2024 9IELTS . All Rights Reserved.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Patterns and Trends of Foot and Ankle Injuries in Olympic Athletes: A Systematic Review and Meta-analysis
Siddhartha sharma, mandeep s dhillon, prasoon kumar, rajesh kumar rajnish.
- Author information
- Article notes
- Copyright and License information
Corresponding author.
Received 2020 Jan 28; Accepted 2020 Feb 19; Collection date 2020 May.
Introduction
Foot and ankle injuries in elite athletes can result in decreased performance, absence from sport and prolonged morbidity. There is paucity of data on foot and ankle injuries in Olympics athletes.
We conducted a systematic review of the PubMed and EMBASE databases. Studies in English language that reported the incidence and/or prevalence of foot and ankle injuries in during Olympics games (summer, winter and youth Olympics) were included. Studies in languages other than English, those that looked at injuries other than foot and ankle injuries, studies looking at injuries in non-Olympics events and those looking at Olympics trials were excluded. We determined the injury rates and burden of foot and ankle injuries. We also looked at the patterns and trends of foot and ankle injuries.
A total of 399 foot and ankle injuries from 25 publications were included in the review. Foot and ankle injury rates ranged from 0.09 to 0.42 injuries per athlete-years for summer Olympics and 0.02–0.35 injuries per athlete-years for winter Olympics. Quantitative analysis revealed that foot and ankle injuries contributed to 16.9% of all injuries (95% CI 8.1–31.9%) for summer Olympics and 5.1% of all injuries (95% CI 1.9–12.6%) for winter Olympics; however, a high statistical heterogeneity was noted. The three most common injuries were tendon injuries, ligament injuries and stress fractures. The rates and burden of foot and ankle injuries showed a declining trend.
Conclusions
Foot and ankle injuries are an important cause of morbidity amongst Olympics athletes. The declining trend amongst these injuries notwithstanding, there is a need for a global electronic database for reporting of injuries in Olympics athletes.
Keywords: Olympics, Foot and ankle, Injuries, Meta-analysis, Sport, Injury prevention
The modern Olympics games are considered as the pinnacle of all sporting events and participation has steadily increased ever since their inception in 1896. As is the case with any mass sporting event, sport-related injuries are a major concern, both for the athletes as well as the organizers [ 1 – 3 ]. It has been shown that foot and ankle injuries can affect athletic performance adversely, result in absence from sport and can also have long-term impact on the athletes’ well-being [ 4 – 6 ]. However, data on foot and ankle injuries in Olympics athletes is scarce. Hence, this study was done to determine the patterns and trends of foot and ankle injuries in Olympic athletes.
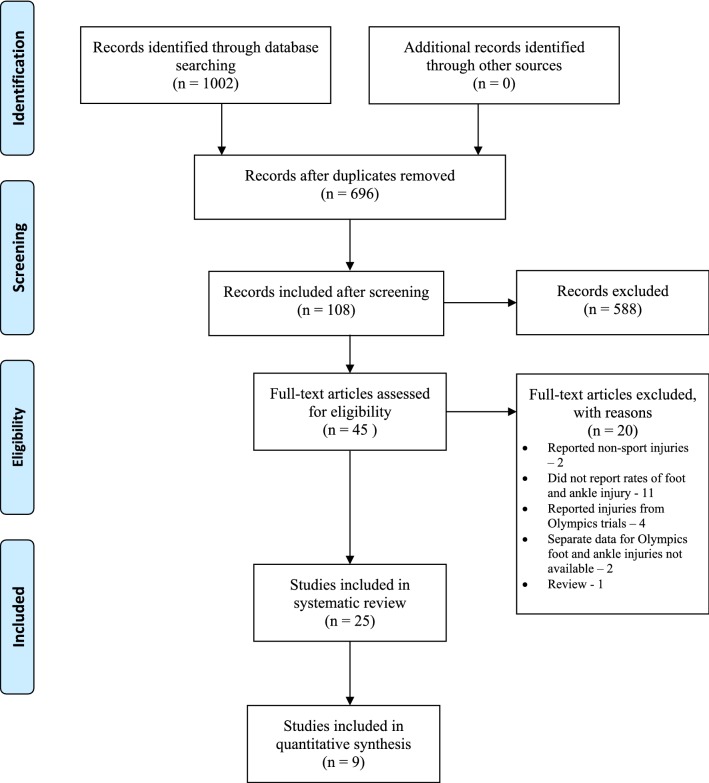
This was a systematic review and meta-analysis, and was done in accordance with PRISMA guidelines [ 7 ].
Search Strategy
The primary search was conducted on the PubMed and EMBASE databases, using a well-defined search strategy that was formulated a-priori (Table 1 ). For secondary search, references of included studies and relevant review articles identified from the primary search were explored.
Search strategy
Inclusion and Exclusion Criteria
Studies in English language that reported the incidence and/or prevalence of foot and ankle injuries in during Olympics games (summer, winter and youth Olympics) were included. Studies in languages other than English, those that looked at injuries other than foot and ankle injuries, studies looking at injuries in non-Olympics events and those looking at Olympics trials were excluded.
Study Selection
Selection of studies for inclusion into the review was done independently by two authors (SS and RR). The titles and abstracts were screened initially and full-texts were subsequently obtained to assess eligibility for inclusion into the review. All discrepancies were resolved by mutual agreement.
Data Extraction
Data was extracted from the included studies by three authors (SS, PK and RR); the following parameters were recorded: (a) country and year of publication (b) total number of athletes included (c) total number of injuries reported (d) total foot and ankle injuries reported (e) age and sex distribution (f) sport-wise distribution (g) specific types of foot and ankle injuries.
Estimation of Injury Rates and Burden of Foot and Ankle Injuries
The incidence rate (IR) for injuries was determined as injuries per athlete-years and was calculated by the following formula:
To ensure uniformity in calculation of IR, the total number of athletes in each Olympic study period was determined from official data provided by the International Olympic Federation. The study period used in the denominator was the period of Olympics games reported by the study authors, if the period was not reported, it was determined from official data provided by the International Olympics Federation.
Incidence rates were calculated for (i) all injuries and (ii) foot and ankle injuries separately. The burden of foot and ankle injuries was calculated from the percentage of foot and ankle injuries (as a function of all injuries) during the study period.
Both qualitative and quantitative analyses were performed. For quantitative analysis, appropriate tables and diagrams were constructed. For quantitative analysis, a random-effects model was used and pooled rates of injuries in summer and winter Olympics were calculated. Heterogeneity was assessed by the I 2 test.
Injury Trends
Line graphs were used to study the trends of overall injury rates, foot and ankle injury rates and percentage of foot and ankle injuries.
Risk of Bias Assessment
Risk of bias in the included studies was assessed independently by two observers (SS and RR) using the NIH case series tool [ 8 ]. The tool consists of 14 items, which was adapted for this review. Discrepancies were resolved by mutual agreement.
Search Results
The results of search have been summarized as per the PRISMA flow diagram (Table 2 ). A total of 1002 records were identified from the searches; 46 full-text articles were obtained and 25 studies were deemed eligible for inclusion in the review.
PRISMA flow diagram for the study
Characteristics of Studies Included
Of the 25 studies included, 13 looked at reported on injuries during summer Olympics, 7 during winter Olympics and 4 during youth Olympics (Fig. 1 ). Whereas the vast majority ( n = 22) of the studies reported on injuries in a single Olympics games period, one study each reported on injuries during two, three and four Olympic games periods. 18 studies reported injuries in all types of sports, whereas 7 studies reported injuries in individual sports only (Table 3 ).
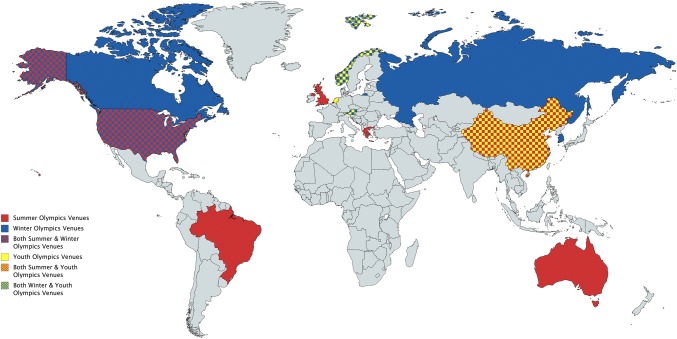
Venues of Olympics games included in the study
Characteristics of studies included in the review
Injury Rates and Burden of Foot and Ankle Injuries in Summer Olympics
Eight studies [ 6 , 9 – 15 ] reported on injuries in all summer Olympics sports (Table 4 ). Of these, 5 studies were deemed unsuitable for calculation of injury rates. Crema et al. [ 10 ] studied only muscle injuries, Elias et al. [ 11 ] studied only plantar fascia and Achilles tendon injuries, Hayashi et al. [ 15 ] studied only bone stress injuries, Jaraya et al. [ 12 ] studied only tendon abnormalities and Keim et al. [ 14 ] reported injury data from a single center. Hence, 3 studies [ 6 , 9 , 13 ] were used to calculate the overall injury rates and foot and ankle injury rates in summer Olympics. The overall injury rate in summer Olympics ranged from 0.4 to 2.4 injuries per athlete-years. The foot and ankle injury rate in summer Olympics ranged from 0.09 to 0.42 injuries per athlete-years. Pooled analysis of injury rates was not done, as the total number of athletes included in study was not thought to be an accurate reflection of all athletes participating in the Olympics, and was, therefore, deemed likely to affect the results. Meta-analysis revealed that foot and ankle injuries contributed to 16.9% of all injuries (95% Confidence Intervals, 8.1–31.9%) (Fig. 2 ). However, the I 2 test revealed very high heterogeneity (98.1%).
Studies that included all Summer Olympics sports
a Injury rates as expressed as the number of injuries per athlete-years
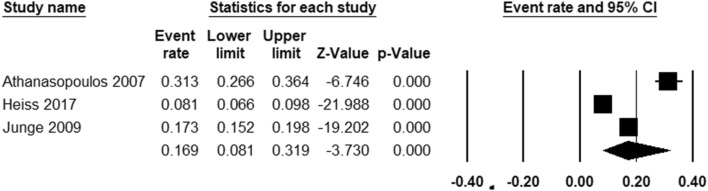
Pooled analysis of percentage of foot and ankle injuries in Summer Olympics
Injury Rates in Winter Olympics
Six studies [ 16 – 21 ] reported on injury rates in all Winter Olympics sports (Table 5 ). The overall injury rates in winter Olympics ranged from 0.74 to 2.81 injuries per athlete-years. The foot and ankle injury rate in winter Olympics ranged from 0.02 to 0.35 injuries per athlete-years. As was the case with studies looking at summer Olympics, pooled analysis of injury rates was not done, as the total number of athletes included in study was not thought to be an accurate reflection of all athletes participating in the Olympics. Meta-analysis revealed that foot and ankle injuries contributed to 5.1% of all injuries (95% Confidence Intervals 1.9–12.6%) (Fig. 3 ). However, the I 2 test revealed very high heterogeneity (92.9%).
Studies that included all Winter Olympics sports
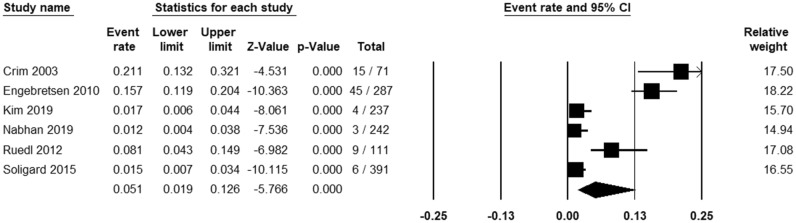
Pooled analysis of percentage of foot and ankle injuries in Winter Olympics
Studies that Included Individual Olympics Sports
Seven studies looked at injuries in individual Olympics sports [ 22 – 28 ]. Of all these, Taekwondo was found to have the highest percentage of foot and ankle injuries (52.1%) [ 22 ], followed by Gymnastics (42%) [ 23 ] and Alpine skiing (33.3%) [ 24 ]. Wrestling had the lowest percentage of foot ankle injuries (3.1%) [ 28 ].
Trends for injury rates could be determined from 2002 to 2018. No definite trend was observed in the overall injury rates. However, it was observed that the foot and ankle injury rates peaked in 2008 and steadily declined thereafter (Fig. 4 ). Trends for burden of foot and ankle injuries could be determined from 1996 to 2018. It was observed that the percentage of foot and ankle injuries peaked in 2004 and steadily declined thereafter (Fig. 5 ).
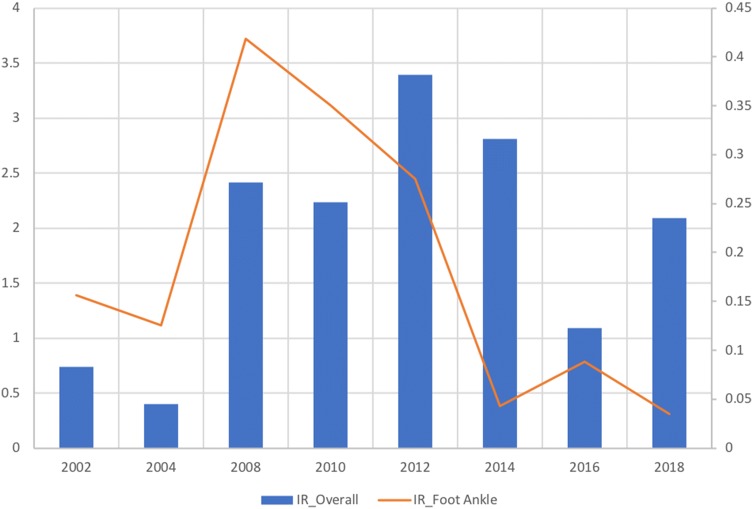
Trends of overall and foot and ankle injury rates in Olympics from 2002 to 2018
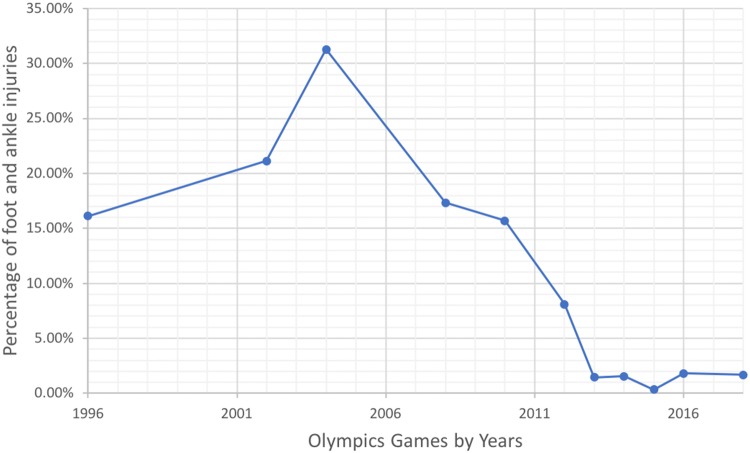
Trends of percentage of foot and ankle injuries in Olympics from 1996 to 2018
Patterns of Foot and Ankle Injuries
A total of 399 foot and ankle injuries were identified in this study. Of all the foot and ankle injuries tendon injuries ( n = 176, 44%), ligament injuries ( n = 94, 24%) and stress fractures ( n = 82, 21%) were the three most common foot and ankle injuries (Fig. 6 a).
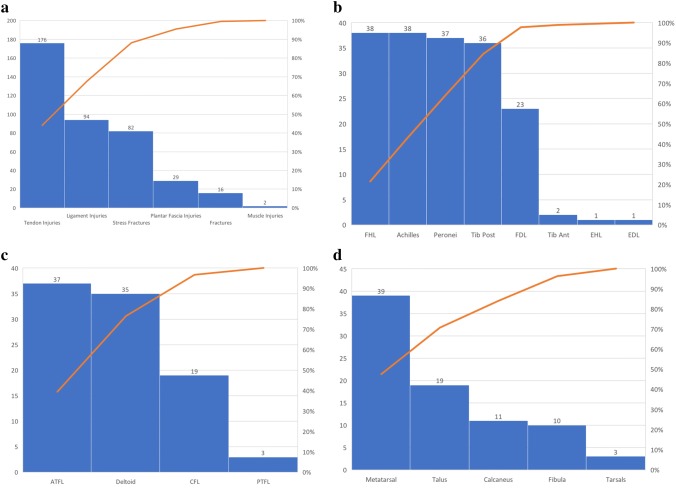
Pareto chart of foot and ankle injuries in the study. a Patterns of all foot and ankle injuries. b Patterns of tendon injuries. c Patterns of ligament injuries. d Patterns of stress fractures
Of all the tendon injuries, injuries to the Achilles tendon and flexor hallucis longus tendon were most common ( n = 38, 21.6%), followed by peroneal (longus and brevis) tendon ( n = 37, 21%) and tibialis posterior tendon ( n = 36, 20.5%) injuries. Acute fractures accounted for approximately 4% of all injuries (Fig. 6 b).
Of all the ligament injuries, injuries to the anterior talofibular ligament ( n = 37, 39.4%) were most common, followed by deltoid ( n = 35, 37.2%) and calcaneofibular ( n = 19, 20.2%) ligament injuries (Fig. 6 c).
Of all the stress fractures, those involving the metatarsal bones ( n = 39, 47.6%) were most common, followed by those involving the talus (n = 19, 23.2%) and calcaneus ( n = 11, 13.4%) bones (Fig. 6 d).
Risk of Bias Assessment (Table 6 )
Studies that included individual Olympics sports
Of the 25 studies included in the review, 13 were rated as Good and 8 as Fair as per the NIH case series tool. 4 studies were deemed as Poor as the study authors felt that they were not representative of an ideal Olympics cohort. Of these, Crema et al. [ 10 ] studied only imaging detected muscle injuries, Elias et al. [ 11 ] studied only plantar fascia and Achilles tendon injuries, Jarraya et al. [ 12 ] studied only tendon injuries and Hayashi et al. [ 15 ] studied only bone-stress injuries.
Foot and ankle injuries in elite athletes can be devastating, and can often result in prolonged absence from sport. It has been estimated that foot and ankle injuries account for 27% of all injuries in elite collegiate athletes and 21% of these injuries result in missed time [ 5 ]. Furthermore, many foot and ankle injuries tend to be recurrent, and can adversely affect the overall athletic performance and quality of life (Table 7 ).
Authors assessment of risk of bias (NIH case series tool)
CD can’t determine, NR not reported
a Reasons for overall assessment as ‘Poor’ reported in the Risk of Bias section
In a systematic review, Fong et al. [ 4 ] studied injury patterns and rates of ankle injuries and ankle sprains in sports. They reported that the prevalence of ankle injuries was highest in aeroball and wall climbing. However, the incidence of ankle injuries was highest in hurling and camogie, followed by rugby. Ankle sprains were the most common injuries, followed by fractures. Rugby had the overall highest incidence of ankle sprains.
Data on foot and ankle injuries in Olympics athletes is sparse and limited to a few observational studies [ 6 , 11 , 15 ]. To the best of our knowledge, this is the first study to evaluate the patterns and trends of foot and ankle injuries in Olympics athletes. We noted that summer Olympics had higher injury foot and ankle rates and accounted for higher percentage of all injuries as compared to winter Olympics. We believe that this may be due to a number of reasons. Foremost is the fact that winter Olympics athletes tend to use specialized boots and sport-gear, that may result in lower injury to the foot and ankle. On the other summer Olympics athletes tend to use shoes rather than boots, which may not be as protective for the foot and ankle. Additionally, many summer Olympics sports such as Taekwondo and Rugby are contact sports, which involve direct injury to the unprotected foot and ankle, thereby accounting for higher injury rates [ 22 , 25 ]. Finally, summer Olympics include a number of track and field sports, which are associated with higher rates of foot and ankle injuries.
We also noted that the rates and burden of foot and ankle injuries in Olympics showed a steady decline. Although it is hard to pin point, the reasons for this trend, we believe that this may be attributable to advances in protective gear, advancements in our understanding in injury patho-mechanics implementation of injury prevention protocols.
The most common foot and ankle injuries noted in our study were those involving tendons, ligaments and stress fractures. This is line with the findings of Fong et al. [ 4 ]. Elite athletes tend to push themselves to the limit, which may result in chronic injuries to the tendons and ligaments. Acute injuries can also ensue in background of such chronic injuries.
During the conduct of this study, we noted a few issues with the available literature on injuries in Olympics. Foremost is the lack of a universal database to ensure that all injuries sustained in Olympics athletes are recorded and reported. We noted that publications on injuries in Olympics tend to come from researchers and clinicians involved in the Olympics polyclinics set up by host countries [ 6 , 9 , 10 , 12 , 15 , 18 ], or from researchers associated with national Olympics teams [ 19 , 29 ]. Furthermore, the available data are often incomplete, as players from the developed nations often do not utilize the services of Olympics polyclinics, and tend to report to their individual medical teams. On the other hand, athletes from developing nations tend to utilize the services of Olympics polyclinics more often, and many of them tend to present with chronic rather than acute ailments [ 9 , 30 ]. In view of these, the estimation of true injury incidence rates remains problematic. To overcome these problems, we would like to put forth the suggestion of a uniform injury reporting electronic database under the aegis of the International Olympics Committee. We feel that this step would go a long way in improving our understanding and prevention of injuries in Olympics.
There are a few limitations of this study. Owing to the nature of published data available, we did not perform meta-analysis of injury rates, nor were we able to determine sport-specific foot and ankle injury rates. In addition, we acknowledge that we may have underestimated the injury rates and burden, owing to the fact that all injuries may not have been reported in the first place. In addition, the overall quality of studies included in the study was moderate. Finally, the high statistical heterogeneity in estimation of pooled burden of foot and ankle injuries indicates that these results should be interpreted with caution.
These limitations notwithstanding, there are several strengths of this study. We strictly adhered to the PRISMA guidelines, used a well-defined search strategy that was formulated a-priori and strictly adhered to our study protocol.
Foot and ankle injuries account for approximately 5% of all injuries in winter Olympics and 16% of all injuries in summer Olympics. The most common foot and ankle injuries are ligament and tendon injuries. Rates of foot and ankle injuries have shown a steady decline. The declining trend notwithstanding, there is a need for a universal database for reporting of foot and ankle injuries in Olympics.

Compliance with Ethical Standards
Conflict of interest.
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- 1. Collier R. Providing medical services at Olympics a huge task. CMAJ. 2012;184(13):E703–704. doi: 10.1503/cmaj.109-4268. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. McCaffery M. Preparing for the worst: Medical services at the Calgary Olympics. CMAJ. 1988;138(2):151–153. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Gunby P. Postmortem on Winter Olympics medical care. JAMA. 1980;244(3):224–225. doi: 10.1001/jama.1980.03310030006002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Fong DT-P, Hong Y, Chan L-K, Yung PS-H, Chan K-M. A systematic review on ankle injury and ankle sprain in sports. Sports Medicine. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Hunt KJ, Hurwit D, Robell K, Gatewood C, Botser IB, Matheson G. Incidence and epidemiology of foot and ankle injuries in elite collegiate athletes. American Journal of Sports Medicine. 2017;45(2):426–433. doi: 10.1177/0363546516666815. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Heiss R, Guermazi A, Jarraya M, Engebretsen L, Hotfiel T, Parva P, et al. Prevalence of MRI-detected ankle injuries in athletes in the Rio de Janeiro 2016 Summer Olympics. Academic Radiology. 2019;26(12):1605–1617. doi: 10.1016/j.acra.2019.02.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Medicine. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Quality Assessment Tool for Case Series Studies - NHLBI, NIH [Internet]. Retrieved 13 March, 2017, from https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/case_series .
- 9. Athanasopoulos S, Kapreli E, Tsakoniti A, Karatsolis K, Diamantopoulos K, Kalampakas K, et al. The 2004 Olympic Games: Physiotherapy services in the Olympic Village polyclinic. British Journal of Sports Medicine. 2007;41(9):603–609. doi: 10.1136/bjsm.2007.035204. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Crema MD, Jarraya M, Engebretsen L, Roemer FW, Hayashi D, Domingues R, et al. Imaging-detected acute muscle injuries in athletes participating in the Rio de Janeiro 2016 Summer Olympic Games. British Journal of Sports Medicine. 2018;52(7):460–464. doi: 10.1136/bjsports-2017-098247. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Elias DA, Carne A, Bethapudi S, Engebretsen L, Budgett R, O’Connor P. Imaging of plantar fascia and Achilles injuries undertaken at the London 2012 Olympics. Skeletal Radiology. 2013;42(12):1645–1655. doi: 10.1007/s00256-013-1689-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Jarraya M, Crema MD, Engebretsen L, Teytelboym OM, Hayashi D, Roemer FW, et al. Epidemiology of imaging-detected tendon abnormalities in athletes participating in the Rio de Janeiro 2016 Summer Olympics. British Journal of Sports Medicine. 2018;52(7):465–469. doi: 10.1136/bjsports-2017-098187. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Junge A, Engebretsen L, Mountjoy ML, Alonso JM, Renstrom PAFH, Aubry MJ, et al. Sports injuries during the Summer Olympic Games 2008. American Journal of Sports Medicine. 2009;37(11):2165–2172. doi: 10.1177/0363546509339357. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Keim ME, Williams D. Hospital use by Olympic athletes during the 1996 Atlanta Olympic Games. Medical Journal of Australia. 1997;167(11–12):603–605. doi: 10.5694/j.1326-5377.1997.tb138910.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Hayashi D, Jarraya M, Engebretsen L, Crema M, Roemer F, Skaf A, et al. Epidemiology of imaging-detected bone stress injuries in athletes participating in the Rio de Janeiro 2016 Summer Olympics. British Journal of Sports Medicine. 2018;52(7):470–474. doi: 10.1136/bjsports-2017-098189. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Crim JR. Winter sports injuries. The 2002 Winter Olympics experience and a review of the literature. Magnetic Resonance Imaging Clinics of North America. 2003;11(2):311–321. doi: 10.1016/S1064-9689(03)00027-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Engebretsen L, Steffen K, Alonso JM, Aubry M, Dvorak J, Junge A, et al. Sports injuries and illnesses during the Winter Olympic Games 2010. British Journal of Sports Medicine. 2010;44(11):772–780. doi: 10.1136/bjsm.2010.076992. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Kim D-S, Lee Y-H, Bae KS, Baek GH, Lee SY, Shim H, et al. PyeongChang 2018 Winter Olympic Games and athletes’ usage of “polyclinic” medical services. BMJ Open Sport & Exercise Medicine. 2019;5(1):e000548. doi: 10.1136/bmjsem-2019-000548. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Nabhan D, Windt J, Taylor D, Moreau W. Close encounters of the US kind: illness and injury among US athletes at the PyeongChang 2018 Winter Olympic Games. British Journal of Sports Medicine. 2019 doi: 10.1136/bjsports-2018-100015. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Ruedl G, Schobersberger W, Pocecco E, Blank C, Engebretsen L, Soligard T, et al. Sport injuries and illnesses during the first Winter Youth Olympic Games 2012 in Innsbruck, Austria. British Journal of Sports Medicine. 2012;46(15):1030–1037. doi: 10.1136/bjsports-2012-091534. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Soligard T, Palmer D, Steffen K, Lopes AD, Grant M-E, Kim D, et al. Sports injury and illness incidence in the PyeongChang 2018 Olympic Winter Games: A prospective study of 2914 athletes from 92 countries. British Journal of Sports Medicine. 2019;53(17):1085–1092. doi: 10.1136/bjsports-2018-100236. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Altarriba-Bartes A, Drobnic F, Til L, Malliaropoulos N, Montoro JB, Irurtia A. Epidemiology of injuries in elite taekwondo athletes: Two Olympic periods cross-sectional retrospective study. British Medical Journal Open. 2014;4(2):e004605. doi: 10.1136/bmjopen-2013-004605. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Edouard P, Navarro L, Branco P, Gremeaux V, Timpka T, Junge A. Injury frequency and characteristics (location, type, cause and severity) differed significantly among athletics ('track and field’) disciplines during 14 international championships (2007–2018): Implications for medical service planning. British Journal of Sports Medicine. 2019;54:159–167. doi: 10.1136/bjsports-2019-100717. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Ekeland A, Dimmen S, Lystad H, Aune AK. Completion rates and injuries in alpine races during the 1994 Olympic Winter Games. Scandinavian Journal of Medicine and Science in Sports. 1996;6(5):287–290. doi: 10.1111/j.1600-0838.1996.tb00472.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Fuller CW, Taylor A, Raftery M. 2016 Rio Olympics: An epidemiological study of the men’s and women’s Rugby-7s tournaments. British Journal of Sports Medicine. 2017;51(17):1272–1278. doi: 10.1136/bjsports-2016-097301. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Junge A, Dvorak J, Graf-Baumann T, Peterson L. Football injuries during FIFA tournaments and the Olympic Games, 1998–2001: Development and implementation of an injury-reporting system. American Journal of Sports Medicine. 2004;32(1 Suppl):80S–S89. doi: 10.1177/0363546503261245. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Mountjoy M, Miller J, Junge A. Analysis of water polo injuries during 8904 player matches at FINA World Championships and Olympic games to make the sport safer. British Journal of Sports Medicine. 2019;53(1):25–31. doi: 10.1136/bjsports-2018-099349. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Shadgan B, Feldman BJ, Jafari S. Wrestling injuries during the 2008 Beijing Olympic Games. American Journal of Sports Medicine. 2010;38(9):1870–1876. doi: 10.1177/0363546510369291. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Nabhan D, Walden T, Street J, Linden H, Moreau B. Sports injury and illness epidemiology during the 2014 Youth Olympic Games: United States Olympic Team Surveillance. British Journal of Sports Medicine. 2016;50(11):688–693. doi: 10.1136/bjsports-2015-095835. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Engebretsen L, Soligard T, Steffen K, Alonso JM, Aubry M, Budgett R, et al. Sports injuries and illnesses during the London Summer Olympic Games 2012. British Journal of Sports Medicine. 2013;47(7):407–414. doi: 10.1136/bjsports-2013-092380. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. van Beijsterveldt AM, Thijs KM, Backx FJ, Steffen K, Brozičević V, Stubbe JH. Sports injuries and illnesses during the European Youth Olympic Festival 2013. British Journal of Sports Medicine. 2015;49(7):448–452. doi: 10.1136/bjsports-2014-094035. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Ruedl G, Schnitzer M, Kirschner W, et al. Sports injuries and illnesses during the 2015 Winter European Youth Olympic Festival. British Journal of Sports Medicine. 2016;50(10):631–636. doi: 10.1136/bjsports-2015-095665. [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Steffen K, Moseid CH, Engebretsen L, et al. Sports injuries and illnesses in the Lillehammer 2016 Youth Olympic Winter Games. British Journal of Sports Medicine. 2017;51(1):29–35. doi: 10.1136/bjsports-2016-096977. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (1.9 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

Sports Related Foot Injuries
May 02, 2023
40 likes | 52 Views
Sports-related foot and ankle injuries are a common occurrence among athletes of all levels, and can range from minor sprains to severe fractures. The feet and ankles are complex structures that are composed of bones, joints, ligaments, tendons, and muscles, which are all susceptible to injury. The most common types of sports-related foot and ankle injuries include sprains, strains, fractures, and tendinitis.
Share Presentation

Presentation Transcript
Sports-Related Foot and Ankle Injuries Sports-related foot and ankle injuries are a common occurrence among athletes of all levels, and can range from minor sprains to severe fractures. The feet and ankles are complex structures that are composed of bones, joints, ligaments, tendons, and muscles, which are all susceptible to injury. The most common types of sports-related foot and ankle injuries include sprains, strains, fractures, and tendinitis. Sprains Sprains occur when the ligaments that connect the bones in the foot and ankle are stretched or torn. Ligaments are strong, fibrous connective tissues that provide stability to the joints. Sprains can occur from a variety of causes, including landing on an uneven surface, twisting or rolling of the ankle, or sudden impact. Symptoms of a sprain include pain, swelling, and difficulty bearing weight on the affected foot. Treatment for a recurrent ankle sprain typically includes rest, ice, compression, and elevation (RICE) to reduce swelling and pain, as well as physical therapy to regain strength and range of motion in the affected joint.
Strains Strains occur when the muscles or tendons in the foot or ankle are stretched or torn. Tendons are connective tissues that attach muscles to bones, while muscles are responsible for movement. Strains can occur from overuse, improper technique, or a sudden impact. Symptoms of a strain include pain, stiffness, and weakness in the affected area. Treatment for a strain typically includes rest, ice, and physical therapy to regain strength and range of motion in the affected muscle or tendon. Fractures Fractures occur when a bone in the foot or ankle is broken. Fractures can occur from a variety of causes, including direct impact, twisting or rolling of the ankle, or overuse. Symptoms of a fracture include severe pain, swelling, and difficulty bearing weight on the affected foot. Treatment for a stress fracture typically includes immobilization of the affected bone using a cast or brace, and physical therapy to regain strength and range of motion in the affected joint. Tendinitis Tendinitis is an overuse injury that occurs when the tendons in the foot or ankle become inflamed. Tendinitis can occur from repetitive motions, such as running or jumping, or from improper technique. Symptoms of tendinitis include pain, swelling, and stiffness in the affected area. Treatment for tendinitis typically includes rest, ice, and physical therapy to regain strength and range of motion in the affected tendon. Other Factors Related to Injuries
In addition to these common injuries, there are also a number of other conditions that can affect the feet and ankles of athletes. These include stress fractures, blisters, and plantar fasciitis, which is an overuse injury that affects the connective tissue on the bottom of the foot. Preventing sports-related foot and ankle injuries is key to maintaining good health and staying active in sports. Proper warm-up and cool-down, as well as stretching and conditioning exercises, can help to prevent injuries. It is also important to wear proper footwear and use proper technique when participating in sports. Additionally, it’s important to be aware of the signs and symptoms of injury and seek treatment as soon as possible if an injury occurs. Sports-related foot and ankle injuries are a common occurrence among athletes of all levels. These injuries can range from minor sprains to severe fractures, and can occur from a variety of causes, including overuse, improper technique, or sudden trauma. Common types of sports- related foot and ankle injuries include sprains, strains, fractures, and tendinitis. Treatment for these injuries typically includes rest, ice, and physical therapy to regain strength and range of motion in the affected joint or muscle. By taking steps to prevent injuries, such as proper warm-up and cool-down, stretching and conditioning exercises, wearing proper footwear, and using proper technique, athletes can reduce their risk of developing sports- related foot and ankle injuries. Additionally, it is important to seek treatment as soon as possible if an injury does occur, in order to minimize the risk of further damage and promote a quick recovery. Preventing and Treating Sports-Related Injuries Physical therapists, athletic trainers, and sports medicine physicians are all valuable resources for preventing and treating sports-related foot and ankle injuries. Above all else, a Podiatrist near you is the best option since they can provide guidance on proper technique, design a rehabilitation program to help you regain strength and range of motion, and provide education on injury prevention and management. In conclusion, sports-related foot and ankle injuries can happen to anyone living an active lifestyle, and they can range from minor sprains to severe fractures. It is important for athletes to be aware of the signs and symptoms of injury and to seek treatment as soon as possible. By taking steps to prevent injuries, such as proper warm-up and cool-down, stretching and conditioning exercises, wearing proper footwear, and using proper technique, athletes can reduce their risk of developing sports-related foot and ankle injuries. With the right care and attention, sports-related foot and ankle injuries can be managed, and athletes can return to their sport and continue to enjoy the many benefits it provides. Visit Ankle and Foot Centers of America now.
- More by User
Sports-Related Eye Injuries
960 views • 14 slides

Sports Injuries
Sports Injuries. Lucy. Risk. When you take up a sport, there’s always a worry that you might hurt yourself. Some sporting activities are more dangerous than others. A variety of factors influence how safe you’ll be. These include: Environment Weather Equipment
1.28k views • 15 slides
Sports Injuries. Andrew O’Brien Tom Milligan. Scenario. A 40 year old male is asked to play in a work 5 a-side football match. He hasn ’ t played for a number of years but used to play regular 5 a side in his twenties.
880 views • 31 slides
sports injuries
Sports injuries are injuries that occur in athletic activities. They can result from acute trauma, or from overuse of a particular body part.
379 views • 12 slides
SPORTS INJURIES
SPORTS INJURIES. David C. Koronkiewicz, D.O. Iu goshen Orthopedics & Sports Medicine. Indiana Osteopathic Association 32 nd Annual Winter Update December 6,2013. Sports Injuries-Outline. Overview Types of injuries Prevention Specific injuries. Statistics.
5.75k views • 112 slides

Sports Injuries . By: Andrew Brawner. Audience. My audience will target seniors to juniors in high school. Primarily used for a sports medicine class. This Power Point covers the basics of each injury, and its treatment. Injuries Covered. Turf Toe Quad Strain/Tear
567 views • 23 slides

Sports Injuries. Fred Battee Iv. What is a sports injury. Injury caused when playing a sport Often due to overuse At times could be traumatic. Injuries from Overuse. Runner’s Knee Shin Splints Tennis Elbow Shoulder Problem. Runner’s Knee. - Chondromalacia patellae
436 views • 20 slides

Sports Injuries. Learning Objectives: To understand how proper preparation prior to performance can reduce the chance of injury. To understand how to recover more quickly from intense exercise. To understand the specialised techniques used to recover from specific sports-related injuries.
1.04k views • 33 slides

Sports Injuries. INTRINSIC AND EXTRINSIC FACTORS. INTRODUCTION. When participating in any sport, injury is a common occurrence. All types of injuries can be categorized as either: INTRINSIC -- the physical aspect of the athletes body that can cause injury
595 views • 8 slides
Sports Injuries. BED SES UNIT 15. A little something to get you started http://www.youtube.com/watch?v=I3SrLubLKAo http://www.youtube.com/watch?v=fJ_6QqLP_pw&feature=related. Learning outcomes. Know and describe the classification of injuries in relation to time
264 views • 12 slides

Management of Common Sports-related Injuries About the Foot and Ankle
Management of Common Sports-related Injuries About the Foot and Ankle. Robert B. Anderson, MD Kenneth J. Hunt, MD Jeremy J. McCormick, MD. J Am Acad Orthop Surg 2010;18: 546-556. Stewart Morrison Orthopaedic Registrar Western Health June 2011.
346 views • 18 slides

Sports-Related Hand and Wrist Injuries
Sports-Related Hand and Wrist Injuries . Matthew Close, DO Primary Care Sports Fellow Steadman Hawkins Sports Symposium June 10 th , 2011. Objectives. Fingers Thumb Wrist Carpals, radius, ulna. Fractures Dislocations Tendon Injuries Ligament Injuries. Hand Examination. Inspection
1.92k views • 35 slides

Sports injuries
Sports injuries. Chapter overview. Classifying and managing injuries • Classifying sports injuries page 259 • Soft-tissue injuries page 263 • Hard-tissue injuries page 267 • First aid page 270 Injury rehabilitation • Rehabilitation page 276
1.14k views • 53 slides

Sports Injuries. Dr Christopher Tong Sports Medicine Specialists 8/F AON China Building 29 Queens Road Central Hong Kong. Today’s talk. Overview of sports medicine Review of anatomy General principles of sports injuries management including clinical examination lower limb injuries.
784 views • 38 slides

Peeled Orange has a unique collection of Massage Liniments for sports injuries to help speed up the healing process and aid in a quick physical recovery
103 views • 6 slides

Sports related Injuries and Treatments in koramangala
Best Sports Medicine doctor in Koramangala. Dr.Rewat Laxman is one of the Best Doctor for Sports related Injuries - Treatments in Bangalore and he is specializes in Knee replacement ,Joint replacement and other Orthopaedic treatments. To Know More, Click Here, http://boneandjointconsult.com/sports-injuries-treatments/
188 views • 14 slides
SPORTS INJURIES. Dan Muse, MD Brockton Hospital. TRAUMATIC BRAIN INJURIES. TRAUMATIC BRAIN INJURIES. Any injury to the brain caused by direct force to the head.
997 views • 87 slides
Sports injuries and its related first aid
The most common methods of first aid approached for injuries like strains and sprains are Rest, Ice, Compression and Elevation (RICE).
63 views • 3 slides
Go to a Physiotherapist for Sports Related Injuries
Whitehorse Physiotherapy is one of the leading physiotherapy centers that works with a team of specialists who have got years of experience and knows everything about Whitehorse pain relief and other kinds of physiotherapy treatment. So, if you are interested and want to take physiotherapy treatment from Whitehorse Physiotherapy, visit the website of this center and book an appointment.
34 views • 2 slides

Can Sports-related Injuries Lead to Premature Ejaculation
Premature ejaculation is a common sexual disorder that affects many men around the world. It is characterized by the inability to delay ejaculation during sexual intercourse, causing distress and frustration. While there are various factors that can contribute to premature ejaculation, one aspect that is often overlooked is the potential link between sports-related injuries and this condition.
110 views • 10 slides

Sport-Related Foot Injuries How to Prevent Them
Are you passionate about sports but concerned about potential foot injuries? Sky Podiatry understands how important it is to maintain optimal foot health to ensure you stay active and injury-free. Our podiatrists at our foot clinic in Mowbray are committed to keeping you at the top of your game as the leading foot clinic in the region.
61 views • 4 slides

What are the common Sports-Related Shoulder Injuries
AOSM is a popular med-clinic that provides treatment for all shoulder injuries. Here, you will get treatment form the best shoulder surgeons.
89 views • 7 slides
SPORTS INJURIES OF ANKLE AND FOOT original.pptx
sports injuries of ankle and foot is a seminar done by Ms. Megha ck on behalf of completing her master of physiotherapy program during the year 2020-2022 Read less

More Related Content
- 1. SPORTS INJURIES OF ANKLE AND FOOT MEGHA CK GUIDE: DR. HARIPRIYA S
- 2. What is sports injury? • Regular physical activity is probably the most important overall determinant of a population’s health. Unfortunately, physical activity may extract a cost in the form of an activity-related injury • Such injuries are categorized as an acute injury or an overuse injury depending on the mechanism of injury and the onset of symptoms.
- 3. Site Acute injuries Overuse injuries Bone Fracture Periosteal contusion Stress fracture ‘Bone strain’, ‘stress reaction’ Osteitis, periostitis Apophysitis Articular cartilage Osteochondral/chondral fractures Minor osteochondral injury Chondropathy (e.g.softening, fibrillation, fissuring, chondromalacia) Joint dislocation subluxation synovitis osteoarthritis Ligament Sprain/tear (grades I–III) inflammation Muscle Strain/tear (grades I–III) Contusion Cramp Acute compartment syndrome Chronic compartment syndrome Delayed onset muscle soreness Focal tissue thickening/fibrosis
- 4. Tendon Tear (complete or partial) Tendinopathy (includes paratenonitis, tenosynovitis, tendinosis, tendinitis) Bursa Traumatic bursitis Bursitis
- 5. 1.INJURIES TO BONE Ankle and foot fractures • Potts fracture • Avulsion fracture Fractures of the foot • Chopart fracture dislocation • Metatarsal fractures • Stress fractures • Perostitis 2.INJURIES TO ARTICULAR CARTILAGE Osteochondral fracures Osteochondropathy 3.INJURIES TO JOINT Joint dislocation 4.INJURIES TO LIGAMENT Sprains 5.INJURIES TO MUSCLE Strain and Tear Muscle contusion Muscle cramps Compartment syndrome 6.INJURIES TO TENDON Tendon tear Paratenonitis Tenosynovitis Tendinosis 7.INJURY TO BURSA Bursitis
- 6. INJURIES TO BONES Ankle and foot fractures • Ankle injuries are the most common sports-related injury. • An ankle fracture is a break in one or more bones that make up the ankle joint. • People participating in sports such as basketball, football, soccer and skiing are at a high risk of developing ankle fractures. • Common symptoms of an ankle fracture include pain and swelling around the ankle, bruising, tender to touch, inability to walk on the leg, and deformity if the ankle is dislocated. • Treatment varies with the type and severity of the injury.
- 7. Pott's fracture • It is one of a common sporting inversion injury especially in jumping sports (e.g. basketball, volleyball). • They are usually a result of a forced plantarflexion/inversion movement, whereby the complex of ligaments on the lateral side of the ankle is torn by varying degrees • Inversion injuries are also far more common than eversion injuries due to the relative instability of the lateral joint and weakness of the lateral ligaments compared to the medial ligament
- 8. Mechanism of Injury • A Pott’s fracture is a fracture affecting one or both of the malleoli. During activities such as landing from a jump (volleyball, basketball). • when rolling an ankle, a certain amount of stress is placed on the tibia and fibula and the ankle joint. • When this stress is traumatic, and beyond what the bone can withstand, a break in the medial, lateral, or posterior malleolus may occur. • Also, activities involving a sudden change of direction, such as football and rugby, can cause fractures around the malleoli.
- 9. • The fracture often occurs in combination with other injuries such as an inversion injury, a dislocation of the ankle, or other fractures of the foot, ankle, or lower leg • Pott's fractures can vary in location, severity, and type including displaced fractures, un-displaced fractures, bi-malleolar fractures, or compound fractures.
- 10. Clinical Presentation • Persons with a Pott's fracture typically experience a sudden sharp and intense pain around the ankle or lower leg immediately at the time of injury. • Pain is situated at the front, back, inner or outer part of the ankle or lower leg. The patient may have heard a “crack” as well. • Due to the pain, the patient to protect the injury. • In severe cases, weight-bearing may be impossible. • swelling, bruising and pain on firmly touching the affected region of bone .
- 11. • When it is a displaced fracture, an obvious deformity may be noticeable and disability such as is common in Pott's fractures cases
- 12. Diagnosis • careful of the person • increased in diameter of the leg at malleoli level suggests fibular fracture (Keen's sign of Pott's fracture) • Diagnosis of a Pott's Fracture can be confirmed on
- 13. Outcome Measures • Clinical Demerit Points • Maryland Foot Score • Walking speed • Time required to climb a set number of stairs • Short Musculoskeletal Functional Assessment (SMFA) • Ankle-Fracture Outcome of Rehabilitation Measure (A-FORM) • Olerud and Molander (O&M) Questionnaire • Lower Extrimity Functional Scale (LEFS)
- 14. Management • Rest • Displaced Pott’s fracture needs . Post-operatively, protective boot, brace, or a plaster cast, and/or crutches are used for a number of weeks. • Non-displaced fracture - plaster cast immobilization and the use of crutches, followed by the use of a protective boot or brace for a number of weeks. • should perform pain-free flexibility, strengthening, and balance exercises as part of their rehabilitation to ensure an optimal outcome
- 15. • Techniques such as joint mobilization is essential to ensure optimal range of movement and flexibility. • The treatment may also involve electrotherapy, bracing, exercises to improve strength, flexibility and balance, and hydrotherapy.
- 16. Prognosis In the most severe cases of a Pott's fracture, patients usually make a Return to activity or sport can usually take place in a number of weeks to months.
- 17. Avulsion Fractures • An avulsion fracture is where a fragment of bone is pulled away at the ligamentous or tendinous attachment • It can be caused by traumatic traction of the ligament or tendon. • It can occur at numerous sites in the body, but some areas are more sensitive to these types of fractures than others, such as at the ankle which mostly occurs at the lateral aspect of the medial malleolus or in the foot where avulsion fractures are common at the base of the fifth metatarsal, but also at the talus and calcaneus.
- 18. Etiology • The typical cause of injury is an inversion of the foot, generating tension along with the plantar aponeurosis insertion • A to the ankle and foot may cause an avulsion fracture at any of these locations
- 19. Clinical Presentation • Symptoms of an ankle avulsion fracture are very similar to an ankle sprain and it is very difficult to differentiate without an X-ray or an MRI scan. • Pain is usually felt immediately after injury, with an onset of swelling. • Bruising may develop and the patient will have difficulty walking or weight-bearing on the ankle.
- 20. Diagnosis • X-ray may be ordered by the surgeon.Other imaging methods are recommended such as MRI or CT Scan Outcome Measures • Olerud ankle score Medical Management • usually treated conservatively • walking boot or a walking cast can be used, which will remain in situ for 4 to 6 weeks • Surgery is recommended where the bone is displaced from its normal position or where more than 30% of the cubometatarsal joint is involved.
- 21. Physical Therapy Management • Avulsion fractures are often treated as ankle sprains • An inappropriately managed avulsion fractures can lead to significant, long-term functional disability • Most fractures heal well. • Rehabilitation following an avulsion fracture consists of 3 phases; the acute, the recovery, and the functional phase
- 22. Acute phase • Can begin at 2 weeks post-operatively • This phase can include passive range of motion exercises and cryotherapy and is based on the reduction of pain, inflammation, and oedema, while keeping muscle atrophy of the lower limb to a minimum.
- 23. Recovery phase Begins once the goals of the acute phase have been met. This phase can be further divided into 3 stages: Weeks 0-6: active ROM exercises for the toes and the MTP joints, strengthening exercises for the ankle and foot are still premature, however. In week 2, isometric exercises for the dorsiflexors, plantarflexors, invertors, and evertors of the foot, along with active ankle ROM movements can be started. Weeks 6-8: active and passive ROM exercises for the ankle and the subtalar joint with Isometric and isotonic exercises. Exercises for proprioception and proximal strength and control.
- 24. 8-12 weeks: strengthening exercises for the dorsiflexors, plantarflexors, invertors, evertors, long flexors and extensors of the toes are recommended. Full weight-bearing exercises are also permitted.
- 25. FRACTURES OF THE FOOT • Fractures of the calcaneum often occur as a result of a fall from height • Can be painful and may be accompanied by vertebral fractures • The phalanges and metatarsals are commonly injuried by a heavy object falling onto the foot • These fractures do not require reduction or immobilisation
- 26. Calcaneal Fractures • It is a rare type of fracture but has potentially debilitating results.
- 27. Etiology • Tarsal fractures account for 2% of all fractures. • Calcaneal fractures account for 50-60% of all fractured tarsal bones. • Less than 10% present as open fractures. • They generally follow high-energy axial traumas, such as falls from height or motor accidents • 75% of the calcaneus fracture is intra-articular and the prognosis of intra-articular fracture is poor. • 20-25% of the cases with a calcaneal fracture is associated with compression fractures of the lumbar vertebrae.
- 28. • Most patients with calcaneus fractures are young, with the 20-39 age group the most common. • Calcaneal fractures are rare in children
- 29. Mechanism of Injury • Calcaneal fractures are mostly the result of high energy events leading to axial loading of the bone • Predominantly, falls from height and automobile accidents (a foot depressed against an accelerator, brake, or floorboard) are common mechanisms of injury. The talus acting as a wedge causes depression and thus flatten, widen, and shorten the calcaneal body. • Calcaneal fractures can also occur with less severe accidents like an ankle sprain or a stress fracture in runners. • Jumping onto hard surfaces, blunt or penetrating trauma and twisting/shearing events may also cause calcaneus fracture
- 30. Characteristics • Patients will present with diffuse pain, edema, and ecchymosis at the affected fracture site • The patient is not likely able to bear weight, walk, and move the foot. • Swelling in the heel area • Plantar ecchymosis extending through the plantar arch of the foot should raise suspicion significantly. • There may be associated disability of the Achilles tendon, also raising the suspicion of a calcaneus injury. • Skin quality around the heel must be evaluated for tenting and/or threatened skin. This is especially important in the setting of Tongue-type calcaneus fractures
- 31. • Generalized pain in the heel area that usually develops slowly (over several days to weeks): typically for stress fractures • Deformity of the heel or plantar arch: Secondary to the displacement of the lateral calcaneal border outward, there is a possible widening or broadening of the heel.
- 32. Examination • Palpation: Tenderness over calcaneus while squeezing the heel from both sides. A squeeze test is positive in stress fracture of the calcaneus. • A thorough neurovascular examination is a must. For which pulse rate of ipsilateral dorsalis pedis or posterior tibial can be compared to the contralateral limb.If there is any suspicion of arterial injury and prompt further investigation with angiography or Doppler scanning can be done. • Evaluation of all lower extremity tendon function.
- 33. Diagnosis • Radiological examination: X-Ray, CT Scan • Bone scan or MRI • Mondor's Sign • Bohler's Angle • Critical Angle of Gissane
- 35. Classification two general categories • accounts for 25 % of calcaneal fractures • include avulsion injuries • Fractures involving any of the three subtalar articulating surfaces • common results of high force axial loading • An intra-articular fracture can be further classified into:-
- 36. Essex-Lopresti classification: It is based on fracture lines using lateral radiographical images. • Joint depression type: verticle fracture line through the angle of Gissane separating the anterior and posterior portions of the calcaneus. • Tongue type:has the same verticle fracture line as a depression type with another horizontal fracture line running posteriorly, creating a superior posterior fragment
- 37. Sander Classification:It is a widely used classification system 4 types of fracture based on the number and location of the articular fragments. • Type I fractures-nondisplaced • Type II fractures (two articular pieces) • Type III fractures (three articular pieces) • Type IV fractures (four or more articular fragments) - highly comminuted.
- 38. Management • There is no universal treatment or surgical approach to all calcaneal fractures. • Treatment of calcaneal fractures depends on the individual fracture pathoanatomy, accompanying soft-tissue damage, associated injuries, functional demand, and comorbidities of the patient. • The treatment of calcaneus fracture can be divided into two types: operative and non-operative treatment.
- 39. Operative Care • Surgery is the correct form of treatment. • Intraarticular fractures are often treated operatively. • The goal of surgery is to reconstruct the overall shape of the calcaneum and to obtain a good functional result. • Done by open reduction and internal fixation.
- 40. Non-Operative Care • preferable when there is no impingement of the peroneal tendons and the fracture segments are not displaced • despite the presence of a fracture, proper weight-bearing alignment has been adequately maintained and articulating surfaces are not disturbed • Extra-articular fractures are generally treated conservatively
- 41. Physical Therapy management: 3 phases Day -1 to week-1 : Precautions: fixation is not rigid unless the patient has had open reduction and internal fixation. Avoid PROM ROM: AROM of toes, MTP joints and knee. Before casting, do not move the ankle and subtalar joint unless rigidly fixed. Muscle strength: No strengthening to the ankle or foot. Functional activities: NWB stand/pivot transfers and ambulation with assistive devices. Weight Bearing : None.
- 42. 2 Weeks Precautions: fixation is not rigid unless the patient has had open reduction and internal fixation. Avoid PROM ROM: Rigidly fixed and non-rigidly fixed fractures may range the MTP joints only. Muscle strength: Rigidly fixed calcaneal fractures may begin isometric exercises in DF and PF as well as inversion and eversion. Functional Activities: NWB standing/pivot transfers for calcaneus fractures. Weight bearing: Calcaneal fractures are NWB.
- 43. 4-6 Weeks Precautions: All calcaneal fractures are still in a NWB short leg cast. ROM: Rigidly fixed fractures are still casted. Continue AROM to the MTP joints as well as isometric exercises of the ankle, PF and DF and inversion and eversion in the cast. Non-rigidly fixed fractures continue AROM at the MTP joint only. The patient is still in the cast. Muscle strength: Rigidly fixed fractures begin isometric exercises to the dorsiflexors and plantar flexors of the ankle and the invertors and evertors in the cast.
- 44. For non-rigidly fixed fractures no strengthening exercises. Functional Activities: Rigidly fixed fractures of the calcaneus and talus may continue partial weight bearing stand/pivot transferes and a three-point gait. Weight bearing: Rigidly fixed fractures may continue toe-touch to partial weight bearing. Non-rigidly fixed fractures are non-weight bearing in a short leg cast.
- 45. Chopart fracture-dislocation A Chopart's fracture-dislocation is a dislocation of the mid-tarsal joints of the foot, often with associated fractures of the calcaneus, cuboid and navicular bone.
- 46. Etiology • Among the uncommon midfoot injuries, Chopart joint dislocations or fracture-dislocations are the most severe injuries • It is usually caused by falls from height, traffic collisions and twisting injuries to the foot as seen in basketball players.
- 47. Characteristics • They are missed or misdiagnosed in up to 41% of cases • The symptoms and signs of a Chopart fracture-dislocation are: • Abnormal position of the forefoot to medial direction • swelling of the dorsum of foot and pain in the midtarsal region when it gets strained
- 48. Diagnosis: Is made on plain radiograph of the foot, although the extent of injury is often underestimated Treatment: Comprises early reduction of the dislocation, and frequently involves open reduction internal fixation to restore and stabilise the talonavicular joint. Open reduction and fusion of the calcaneocuboid joint is occasionally required Physical Therapy Managanement: PT intervention should begin as soon as possible • maintain surrounding muscular strength and range of motion • maintain functional independence as much as is possible • prevent secondary complications • effective cast care advice and mobility progression Prognosis: With prompt treatment, particularly open reduction, and early mobilisation the outcome is generally good
- 49. Metatarsal Fractures A metatarsal bone fracture is a complete or incomplete break in one of the five metatarsal bones in each foot
- 50. Etiology • The majority of the metatarsal fractures sustained from sport is from soccer (73%) • 5 to 6% of all fractures treated in primary care are metatarsal fractures • are the most common injuries of the foot • The distribution of the fractures looks as follow First metatarsal: 5% Second metatarsal: 12% Third metatarsal: 14% Fourth metatarsal: 13% Fifth metatarsal: 56% Multiple metatarsal fractures: 15,6%
- 51. • Athletes, individuals who are obese, and individuals with osteoporosis or rheumatoid arthritis or diabetes have an increased risk of developing metatarsal fractures • It also appears in sports like jogging, ballet, gymnastics, and high-impact aerobic activities.Shoe shock attenuation can prevent metatarsal stress fractures • The act of repetitive cyclic loading, especially in the setting of a young athlete or military recruit, can lead to a chronic overloading predisposing one to a stress reaction and ultimately fracture.
- 52. Characteristics • Painful swelling • Axial pressure pain Diagnosis • Acute metatarsal fracture • Fractures of the proximal first through fourth metatarsals • A Fracture of the unfused fifth metatarsal base apophysis • Acute fractures of the proximal fifth diaphysis • Jones fracture • Stress fractures
- 53. Physical Therapy Management • first days are protection, rest, ice, compression and elevation important until the swelling is stabilized • joint mobilizations • electrotherapy • hydrotherapy • later on excercises to increase strength, flexibility and balance.
- 54. Stress fractures A stress fracture is a fatigue-induced bone fracture caused by repeated stress over time. stress fractures are the result of accumulated injury from repeated submaximal loading, such as running or jumping
- 55. Etiology • 15-20% of overuse injuries are stress fractures. • activities such as marching and running are associated with these types of fractures • occurs especially the second metatarsal
- 56. Perosteitis • commonly seen in football, basketball, soccer, or dance • Periostitis is a condition that many runners are familiar with. It is caused by inflammation of the periosteum, a layer of connective tissue that surrounds bone.
- 57. Causes • A major increase of mechanical stress • The periosteum is an attachment site for several muscles (soleus, flexor digitorum longus, tibialis posterior). Overworking these muscles can create muscular tension and cause irritation at their attachment site on the periosteum • Foot and ankle biomechanical problems, such as uncontrolled or excessive pronation.
- 58. symptoms • Bone tenderness, difficulty bearing weight on affected limb • Pain • Stiffness, especially when getting out of bed in morning • Fever and chills • Swelling of tissue around bone • Pus forming if left untreated.
- 59. Physical therapy management Phase 1 Inflammation (until day 10) Phase 2 Proliferation (10 days to 8 weeks) Phase 3 Remodeling (up to one year) Electrotherapy Rest, ice, compression, elevation Posture and gait assessment Technical needs assessment (cane, crutches) Manual therapy Electrotherapy Strengthening, flexibility and proprioception exercises Mechanical stress quantification Taping, as necessary Progressive exercises Mechanical stress quantification and training advice Education about prevention
- 60. JOURNAL NAME Scientific Journal of rehabilitation medicine TITLE AUTHOR Comparative Effects of Impacts and Stainabilities of National Academy of Sports Medicine and Combined Exercises (Neuromuscular and Core Stability) on Functional Characteristics and Balance of Individuals with Unilateral Chronic Ankle Injury (2021) A Mohammadi et.al METHODOLOGY A total of 36 male athlete students suffering from chronic ankle instability voluntarily participated in the present study and were randomly divided into three groups of 12: NASM excersices, combined training, and the control group. All the participants’ performance characteristics and dynamic balance were evaluated prior to, after, and four weeks after the exercises. OUTCOME MEASURES Side-to-Side Hop Test, Figure-eight Hop Test, Triple Hop Test, Y balance test CONCLUSION Doing eight weeks of combined training (neuromuscular and core stability) was observed to be significantly more effective, compared with NASM training, in the performance and postural control in patients with chronic ankle instability.
- 61. JOURNAL NAME Orthopedic trauma association TITLE AUTHOR Does formal vs home-based physical therapy predict outcomes after ankle fracture or ankle fracture-dislocation? (2018) C M. Ferguson et.al METHODOLOGY This prospective observational study included patients with operative bimalleolar or trimalleolar ankle fractures with or without dislocation (n=80) at a Level I trauma center. Patients were prescribed PT per the surgeon’s practice pattern. Patient reported functional outcomes at 6 months and complication rates were compared between groups. OUTCOME MEASURES Foot and Ankle Ability Measure (FAAM) Short Form Musculoskeletal Functional Assessment (SFMA) CONCLUSION Comparison of outcomes between patients with operatively treated displaced ankle fractures/dislocations with Formal-PT vs Home-PT showed no difference in SMFA and FAAM scores. These findings suggest patients receiving supervised PT produced a similar outcome to those under routine physician-directed rehabilitation at 6 months.
- 62. INJURIES TO ARTICULAR CARTILAGE Osteochondral fractures • It is an injury to the cartilage and bone in the talus. Etiology: • Twisting injuries in sports of any kind • A fall from a height
- 63. Types : Some injuries will not only affect the cartilage but the bone beneath it. This can cause a bruise or a bone contusion to the bone itself. When associated with a cartilage tear, this becomes more problematic : A piece of bone and cartilage can be partially broken off but have a stable base. : A piece of bone and cartilage can be completely broken off. However, not displaced from its environment or its anatomical place in the bone : A piece of bone and cartilage can be completely broken off and displaced into the ankle joint, causing a severe injury.
- 65. Signs and Symptoms • Chronic swelling • Morning stiffness • A feeling of locking when the ankle moves. A click may also be felt.
- 66. PT Management • joint mobilization • electrotherapy • use of crutches, a walking stick or other walking aid • use of a protective boot • prescription of orthotics or footwear advice • a gradual return to activity program • a gradual return to running program • anti-inflammatory and supplement advice • ankle bracing • the use of heel wedges • the use of a compression bandage • ice or heat treatment • exercises to improve flexibility, strength, core stability and balance • hydrotherapy • education • activity and lifestyle modification advice • biomechanical correction • weight loss advice where appropriate
- 67. osteochondropathy osteochondropathy refers to a group of disease involving both bone and cartilage (softening, fibrillation, fissuring, chondromalacia) Chondromalacia: develops when cartilage deteriorates and softens. if diagnosed early, this condition is reversible with appropriate mediacal and physiotherapy treatment.
- 68. JOURNAL NAME Knee Surgery, Sports Traumatology, Arthroscopy volume TITLE AUTHOR Arthroscopic lift, drill, fill and fix (LDFF) is an effective treatment option for primary talar osteochondral defects (2020) Kaj T. A. Lambers et.al METHODOLOGY Twenty-seven ankles (25 patients) underwent an arthroscopic LDFF procedure for primary fixable talar OCDs. The mean follow-up was 27 months (SD 5). Pre- and post-operative clinical assessments were prospectively performed and patients were radiologically assessed by means of computed tomography (CT) scans pre-operatively and 1 year post-operatively. OUTCOME MEASURES Numeric Rating Scale (NRS), Foot and Ankle Outcome Score (FAOS), Short Form-36 (SF-36) CONCLUSION Arthroscopic LDFF of a fixable primary talar Osteochodral Defects results in excellent improvement of clinical outcomes. The radiological follow-up confirms that fusion of the fragment is feasible in 92%.
- 69. JOURNAL NAME The American Journal of Sports Medicine TITLE AUTHOR Allograft Versus Autograft Osteochondral Transplant for Chondral Defects of the Talus: Systematic Review and Meta-analysis (2021) Filippo Migliorini et.al METHODOLOGY All studies investigating the outcomes of allograft and/or autograft osteochondral transplant as management for osteochondral defects of the talus were accessed. the outcomes and data concerning the rates of failure and revision surgery were also collected and analyzed. OUTCOME MEASURES visual analog scale (VAS), American Orthopaedic Foot and Ankle Society (AOFAS) score, Magnetic Resonance Observation of Cartilage Repair Tissue (MOCART) score CONCLUSION Based on the main findings of the present systematic review, talar osteochondral transplant using allografts was associated with higher rates of failure and revision compared with autografts at midterm follow-up.
- 70. INJURIES TO JOINTS Joint Dislocation A dislocation is when there is an abnormal separation between the bones of a joint. Ankle dislocations often occur along with a break in 1 or more of the ankle bones. In some cases, an ankle dislocation can happen without a break in the ankle bones. In these cases, the ankle dislocation occurs along with a severe ankle sprain. A severe sprain is when the ligaments are torn. Garrick et.al reported that 45% of basketball injuries, 25% of volleyball injuries, and 31% of soccer injuries are to the ankle. Ankle dislocations are more commonly seen in volleyball and basketball because jumping is a fundamental component of these sports.
- 71. Causes • Ankle dislocation results from severe injury to the ankle. • This can happen in a motor vehicle accident. It may also happen while playing sports, especially ones that include jumping. It is more likely to happen when you have your foot pointed down during impact.
- 72. Signs and symptoms • Immediate, severe pain • Swelling and bruising • Soreness to the touch • Inability to put weight on foot
- 73. Diagnosis • physical examination • pain and swelling • X-rays of leg, ankle, and foot to look for bone fractures Medical Management • Pain killers • closed reduction • splints • a cast or boot • emergency surgery
- 74. Physiotherapy Management Weeks 1 - 4 • Start ankle isometrics inside the boot immediately post-op. Do 5 repetitions of 5 second contractions. Repeat this 5x per day. • No ankle range of motion exercises for 4 weeks. • Gait training with crutches to minimize compensations and to enforce touchdown weightbearing status on the surgical leg. Exercises: • Toe curls and toe spreads • Quad-sets with straight-leg raises • Gluteal sets • Well-leg biking • Upper body training
- 75. Weeks 4 - 6: • May start partial weightbearing still using crutches and walking boot. • Can start using AirCast Stirrup splint for sleeping only instead of the walking boot. • Start ankle partial range of motion (ROM) and non-weightbearing to partial weightbearing ankle isotonic exercises. • Soft tissue treatments for swelling, mobility and healing. Weeks 6 - 8: • May start weightbearing as tolerated and progressive weaning of assistive devices (single crutch to cane to no device, if necessary). • Can wean off boot and use AirCast Stirrup instead. • Gait training to normalize movement patterns. • Start to seek full ankle range of motion per patient tolerance and without flare-ups. • Start weightbearing strength and balance exercises. • Begin joint mobilizations to seek full range of motion.
- 76. Weeks 8 - 12: • Increase functional weightbearing exercises and activities. Avoid impact and cutting activities until week 12. • Can start to wean off AirCast Stirrup if the patient has enough dynamic control and stability of the ankle. • Aim for ankle range of motion to be full by week 12. • Continue with mobilizations. Weeks 12 and beyond: • Start sport-specific training. • Increase the intensity of strength, balance, coordination and functional training for gradual return to activities and sports. • Return to specific sports is determined by the physical therapist through functional testing specific to the targeted sport.
- 77. JOURNAL NAME MDPI TITLE AUTHOR Isolated Medial Subtalar Joint Dislocation during Sports Activities: A Systematic Review (2021) Carlo B et.al METHODOLOGY The aim of this study was to verify if a reliable conservative treatment and a specific physiotherapy rehabilitation protocol in isolated medial dislocation of the STJ in athletes.A systematic review of the published literature of the last 11 years was performed by applying the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines using three databases: Pubmed, Scopus, and Web of Science. OUTCOME MEASURES American Orthopedic Foot and Ankle Society (AOFAS) , range of motion (ROM) CONCLUSION A total of 12 studies were included in their review, with a total of 26 athletic patients. Sixteen of them had good results with the correlation between the duration of immobilisation and the outcomes.
- 78. LIGAMENT INJURIES ANKLE SPRAIN
- 79. An ankle sprain is where one or more of the ligaments of the ankle are partially or completely torn. Ankle sprains are most common in basketball – with 45 percent. Soccer accounts for another 31 percent of ankle sprains, and volleyball 25 percent
- 80. Epidemiology • An ankle sprain is a common injury. • Inversion-type, lateral ligament injuries represent approximately 85% of all ankle sprains. • The incidence of ankle sprain is highest in sports populations. • Poor rehabilitation after an initial sprain increases the chances of this injury recurrence. • A meta-analysis by Doherty et al, found that indoor sports carry the greatest risk of ankle sprain with an incidence of 7 per 1,000 cumulative exposures. • Severe ankle sprains occur commonly in basketball players. • Recurrence rates amongst basketball players is reported to be greater than 70%.
- 81. Clinically Relevant Anatomy • Of the lateral ankle ligament complex the most frequently damaged one is the anterior talofibular ligament (ATFL) • On the medial side the strong, deltoid ligament complex is injured with forceful "pronation and rotation movements of the hindfoot • The stabilising ligaments of the distal tibio-fibular syndesmosis are the anterior-inferior, posterior- inferior, and transverse tibio-fibular ligaments, the interosseous membrane and ligament, and the inferior transverse ligament. • A syndesmotic (high ankle) sprain occurs with combined external rotation of the leg and dorsiflexion of the ankle.
- 82. Risk Factors • Several intrinsic and extrinsic risk factors predispose an athlete to chronic ankle instability • The most common risk factor is previous history of sprain • A previous sprain may compromise the strength and integrity of the stabilisers and interrupt sensory nerve fibres • Sex, height, weight, limb dominance, postural sway and foot anatomy are intrinsic. • Extrinsic risk factors may include taping, bracing, shoe type, competition duration and intensity of activity
- 83. Mechanism of Injury • usually occur during a rapid shift of body center of mass over the landing or weight-bearing foot • When a ligament tears or is overstretched its previous elasticity and resilience rarely returns • Reports have proposed that the greater the level of plantar flexion the higher the likelihood of sprain • Yeung et al, 1994, in an epidemiological study of unilateral ankle sprains, reported that the dominant leg is 2.4 times more vulnerable to sprain than the non-dominant one. • A less common mechanism of injury involves forceful eversion movement at the ankle injuring the strong deltoid ligament.
- 84. Aspect Mechanism of injury Ligaments Lateral Inversion and plantarflexion anterior talofibular ligament calcaneo-fibular ligament posterior talofibular ligament Medial Eversion posterior tibiotalar ligament tibiocalcaneal ligament tibionavicular ligament anterior tibiotalar ligament High External rotation and dorsiflextion anterior-inferior tibiofibular ligament posterior-inferior tibiofibular ligament transverse tibiofibular ligament interosseous membrane interosseous ligament inferior transverse ligament
- 85. Clinical Presentation • Patient presents with inversion injury or forceful eversion injury to the ankle. May have previous history of ankle injuries or instability. • Able to partial weight-bear only on the affected side. • If patient presents with description of cold foot or paraesthesia, suspect neurovascular compromise of peroneal nerve. • Tenderness, swelling and bruising can occur on either side of the ankle.
- 86. • No bony tenderness, deformity or crepitus present. • Passive inversion or plantar flexion with inversion should replicate symptoms for a lateral ligament sprain. Passive eversion should replicate symptoms for a medial ligament sprain. • Special Tests: +ve Anterior Draw, Talar Tilt or Squeeze Test (depending on the structures involved).
- 87. Differential Diagnosis • The Ottawa Ankle Clinical Prediction Rules are an accurate tool to exclude fractures within the first week after an ankle injury • Impingement • Tarsal Tunnel Syndrome • Sinus Tarsi Syndrome • Cartilage or osteochondral injuries • Peroneal Tendinopathy or subluxation • Posterior Tibial Tendon Dysfunction
- 88. Classification There are numerous grading systems used for the classification of ligament sprains. The traditional grading system for ligament injuries focuses on a single ligament • Grade I represents a microscopic injury without stretching of the ligament on a macroscopic level. • Grade II has macroscopic stretching, but the ligament remains intact. • Grade III is a complete rupture of the ligament.
- 89. Clinical Examination • With an ankle sprain multiple structures may be involved, therefore a full foot and ankle assessment is recommended • including the mechanism of injury, observation of the patient's gait pattern, standing posture and wear on the individual's shoes • Any gross deformity, mal-alignment or atrophy of the musculature should also be observed and noted as well as any oedema and/or ecchymosis. • Palpation is used to feel for the structures that may be involved in the injury, including bone, muscle and ligamentous structures, followed by an active and passive range of movement assessment.
- 90. Physical Therapy Management Mild Ankle Sprain • Natural full recovery within 14 days • Taping and follow up to evaluate healing progression Severe Ankle Sprain • Inflammatory phase, • Proliferative phase, • Early Remodelling, • Late Maturation and Remodelling
- 91. Inflammatory Phase (0-3 days) Reduction of pain and swelling and improve circulation and partial foot support-PRICE (Protection, Rest, Ice, Compression, and Elevation) Foot and Ankle ROM
- 92. Proliferative Phase (4-10 days) Goals:Recovery of foot and ankle function and improved load carrying capacity. Patient education Practise Foot and Ankle Functions Range of Motion Active Stability Motor Coordination Boyce et al found that the use of an Aircast ankle brace for the treatment of lateral ligament ankle sprains produces a significant improvement in ankle joint function compared with standard management with an
- 93. Early Remodelling (11 -21 days) Goals: Improve muscle strength, active (functional) stability, foot/ankle motion, mobility (walking, walking stairs, running). • information about possible preventive measures (tape or brace) • Advice regarding appropriate shoes to wear during sport activities • balance, muscle strength, ankle/foot motion and mobility (walking, stairs, running). • dynamic stability - focusing on balance and coordination exercises. Gradually progress the loading, from static to dynamic exercises, from partially loaded to fully loaded exercises and from simple to functional multi- tasking exercises • Alternate cycled with non-cycled exercises (abrupt, irregular exercises) • Advise wearing tape or a brace during physical activities until the patient is able to confidently perform static and dynamic balance and motor coordination exercises.
- 94. Late Remodelling and Maturation Goals: Improve the regional load-carrying capacity, walking skills and improve the skills needed during activities of daily living as well as work and sports. Practise and adjust foot abilities (functions and activities) Practise motor coordination skills while performing mobility exercises Continue to progress the load-bearing capacity untill the pre-injury load-carrying capacity is reached Encourage the patient to continue practicing at home
- 95. JOURNAL NAME Journal of Taibah University Medical Sciences TITLE AUTHOR Effects of the standard physiotherapy programme on pain and isokinetic ankle strength in individuals with grade I ankle sprain (2018) M Salim et.al METHODOLOGY Seven patients with acute grade 1 ankle sprain were recruited. provided with 7 days of protection, optimal loading, ice, compression, and elevation (POLICE) treatment, and the standard physiotherapy programme consisted of towel stretching and balancing exercises on one leg. pain and isokinetic ankle strengths of the patient's injured and uninjured legs were compared before and after the physiotherapy programme. OUTCOME MEASURES 10-point Visual Analogue Scale (VAS). Ankle strength using an isokinetic dynamometer CONCLUSION Performing the standard physiotherapy programme for 1 week reduces pain and improves the ankle E:I in patients with grade 1 ankle sprain.
- 96. JOURNAL NAME Research squre TITLE AUTHOR Improvement of Mobility, Strength, Stability and Pain in Soccer Players with Recurrent Ankle Sprains Through Myofascial Release, Strength Exercises and Taping: A Randomized Controlled Trial. Allois R et.al METHODOLOGY over 4 weeks, 36 recreationally active male football players randomly allocated to experimental group and control group. outcomes were assessed. The within- subject effect and group interaction were obtained by means of a repeated measures ANOVA. OUTCOME MEASURES range of motion, strength, stability and perceived pain in the ankle joint. CONCLUSION The combination of fascial therapy and eccentric strength training with an isoinertial device improves ankle mobility, strength and stability in footballers with recurrent ankle sprains. The use of taping techniques failed to provide a greater improvement of the study variables when combined with manual therapy and strength techniques.
- 97. INJURIES TO MUSCLE STRAIN/TEAR • An ankle strain is an injury that occurs when ankle muscles and/or their connecting tendons are either stretched beyond their normal limits or torn outright. • Strains may be acute or chronic. • The muscular injury often occurs at the point where the muscle connects to a tendon, and may be a side effect of or coexist with ankle tendonitis • Less common than ankle sprains, ankle strains often occur due to chronic overuse of the ankle. • This type of injury can occur due to activities such as running long distances, repeated hard landings from jumping (such as in basketball layups or volleyball sets), or repeated hard articulations of the ankle, such as going up on tiptoe in ballet or gymnastics.
- 98. Classification • Grade I (mild) strains affect only a limited number of fibers in the muscle. There is no decrease in strength and there is a fully active and passive range of motion. Pain and tenderness are often delayed to the next day. • Grade II (moderate) strains have nearly half of muscle fibers torn. Acute and significant pain is accompanied by swelling and a minor decrease in muscle strength. • Grade III (severe) strains represent the complete rupture of the muscle. This means either the tendon is separated from the muscle belly or the muscle belly is actually torn in 2 parts. Severe swelling and pain and a complete loss of function are characteristic of this type of strain.
- 99. Signs and Symptoms • Swelling, bruising, or redness due to the injury • Pain at rest • Muscle spasms, cramps, and muscle weakness in the ankle • Limited range of motion Risk Factors • Poor athletic conditioning • Muscle and ligament fatigue • Not warming up before activity • Carrying excess weight. • Inappropriate footwear • Prior history of sprains or strains
- 100. Diagnosis • Inspect the affected ankle visually • Palpate the injury site • Diagnostic testing, such as X-ray or magnetic resonance imaging (MRI) Treatment • For Grade 1 and Grade 2 strains- RICE • NSAIDs and acetaminophen • Grade 3 sprains and strains are usually unstable and require longer healing • Casting • Rehabilitation: Patients may need to undergo a series of rehabilitation treatments, such as electrical stimulation and ultrasound, as well as strengthening exercises to help decrease pain • Surgery. In severe and/or chronic strains that do not respond to first-line treatment or rehabilitation, one or more types of surgery may be required
- 101. Muscle Contusion (Bruise) • Athletes in contact sports have many opportunities to get a muscle contusion (bruise). • Contusions are second only to strains as a leading cause of sports injuries • Most contusions are minor and heal quickly, without taking the athlete away from the game. • Severe contusions, however, can cause deep tissue damage and lead to complications that may prevent an athlete from being able to play sports for months.
- 102. Cause • Contusions occur when a direct blow or repeated blows by a blunt object strike part of the body, crushing underlying muscle fibers and connective tissue without breaking the skin. • A contusion can result from falling or jamming the body against a hard surface. Symptoms • hematoma • If tissue damage is extensive, one may also have a broken bone, dislocated joint, sprain, torn muscle, or other injuries. Treatment • To control pain, bleeding, and inflammation, keep the muscle in a gentle stretch position and use the RICE protocol Complications • Compartment Syndrome • Myositis Ossificans
- 103. MUSCLE CRAMPS • Foot cramps are a type of muscle cramp that occurs most often either in the arch of the foot, near the toes, or on the upper part of the foot • These spasms can occur during daily activities or wake a person in the middle of the night. • Like other muscle cramps, foot cramps can cause mild-to-intense pain until the muscle relaxes and the cramping ends. • A gentle massage or stretching exercises can often help the muscle return to a relaxed state. Causes • Low potassium • Overexercising • Dehydration • Overly tight shoes • Nerve damage
- 104. Treatment light stretching and gentle massages. If overexercising is the cause of foot cramps, a person can reduce the amount of time that they spend exercising or decrease the intensity of the exercise. Prevention exercising within a comfortable limit and wearing suitable sports shoes eating a diet rich in vital nutrients, including potassium drinking plenty of fluids to stay hydrated wearing well-fitted shoes changing any medication that is causing muscle cramps, under a doctor’s instructions
- 105. Compartment Syndrome of the Foot • Compartment syndrome is a condition where bleeding or edema develops in an area of the body which is surrounded by non-expandable structures of bone and fascia, increasing the local pressure and causing circulatory disturbance in that space. • Athletes who participate in activities with repetitive motions, such as running, biking, or swimming, are more likely to develop chronic compartment syndrome. Etiology • Incidence of compartment syndrome of the foot is low • The calcaneal compartment seems to be at higher risk for developing compartment syndrome, whereas the interosseous compartments are usually at a lower risk
- 106. • Chronic (exertional) compartment syndrome can develop through over exertion during sporting activity. • The muscles become fatigued and irritated resulting in an inflammatory response and swelling. • Sports like football, motorcross, running, tennis and gymnastics can be risk factors Characteristics • Pain is one of the key symptoms for compartment syndrome • Pain with passive stretching • Pain during active dorsiflexion of the ankle • Increased soreness caused by moving the toes • Pain on palpation or compressing the affected compartments • Swelling and tightness • Pale skin in the area of tissue damage • Sensory deficits caused by neurological injury • Firmness of the involved compartments • Muscle weakness of the intrinsic foot muscles • 5P’s- Pain, Pallor, Paresthesia, Paralysis, Pulselessness
- 107. Medical Management • fasciotomy in order to remove the excess pressure • Complications: chronic pain and hypersensitivity are possible complications and can be difficult to manage. Sometimes claw toes develops Physiotherapy Management • Non-operative treatment is generally not successful • Post-operatively, patients are advised to use ice and anti-inflammatory medication to reduce swelling and to rest. • An exercise programme is given to improve muscle weakness and to stimulate proprioceptive sensors. • Soft tissue massage-to provide lymphatic drainage. • Passive mobilisation of the ankle joint, the metatarsals and phalanges-for increased range of motion and mobility of joints • lower limb stretches. • strenghthening exercises
- 108. JOURNAL NAME American journal of case reports TITLE AUTHOR Acute Exertional Compartment Syndrome with Rhabdomyolysis: Case Report and Review of Literature (2018) Brandon McKinney et.al METHODOLOGY Presented the case of a previously healthy, high-level athlete who presented with the acute onset of unilateral anterior leg pain and foot drop the day after a strenuous workout. He was diagnosed with compartment syndrome and rhabdomyolysis. His management included emergent fluid resuscitation, fasciotomies, debridement of necrotic muscle from his anterior compartment, and delayed primary closure. After six months of intensive outpatient physical therapy, including the use of blood flow restriction treatments, the patient returned to sports. OUTCOME MEASURES VAS- pain assessment CONCLUSION Early diagnosis and proper treatment can resolve Acute Exertional Compartment Syndrome and reduce the pain .
- 109. JOURNAL NAME JCAM TITLE AUTHOR ASTYM versus massage in the treatment of chronic exertional anterior compartment syndrome of the lower leg: a randomized controlled trial (2018) IM Ragab et.al METHODOLOGY The purpose of this study was to compare the effects of Astym therapy and massage in patients with chronic exertional anterior compartment syndrome of the lower leg. OUTCOME MEASURES Visual analog scale (VAS), CONCLUSION ASTYM treatment is more effective than massage therapy in reducing pain, improving overall functional level for patients with ant-CECS.
- 110. INJURIES TO TENDON Tendon Tear • A foot tendon tear happens when one of the tendons in the foot is damaged from sudden injury or overuse • Posterior tibial tendon: The posterior (rear) tibial tendon attaches the calf muscle to the bones of the inside of the foot. It holds up the arch of the foot and supports the foot during walking. A tear to this tendon is usually from a fall. But it can also be injured from overuse. This is most common in athletes who put a lot of stress on the ankle during sports like basketball or soccer. The anterior tibial tendon runs from the shin to the top of the foot. Injuries to this tendon are much less common than to the posterior tibial tendon.
- 111. • Peroneal tendons: Tears in these tendons are usually caused by an ankle sprain or a blow to the ankle. It can also be caused by overuse, usually in athletes who repeat movements that put stress on the ankle. • Achilles tendon: It is the largest tendon in the body. It can tear if sudden high stress is put on it, especially if the calf muscle is stiff or weak and can’t take its share of the stress.
- 112. Symptoms • Pain • Swelling, redness, and warmth • Weakness or loss of function Causes • fall on the foot or sudden pressure on the tendon • repetitive use of the foot and ankle in ways that put stress on the tendon-This is more likely to happen to athletes who put repetitive stress on their ankles • people with high arches have a higher risk of foot tendon tears.
- 113. Diagnosis • examination of the foot • X-ray to check for broken bones and look for other damage • MRI or CT scan
- 114. Treatment • Rest • Ice • NSAID • Brace or cast • Orthotics
- 115. Paratenonitis • Paratenonitis has sometimes also been referred to as ‘peritendinitis’ or ‘paratendonitis’ • commonly found in athletes as a result of overuse injury • Paratenonitis can develop as a result of overuse or repetitive microtrauma • Paratenonitis affects tendons with a paratenon and thus without a synovial sheath e.g. Achilles tendon, patella tendon gluteal tendons, etc. The most common location of paratenonitis is the Achilles tendon. RISK FACTORS • dancers • long-distance runners
- 116. Clinical Features Local pain and swelling, tenderness on palpation along the anatomic course of the tendon and in chronic stages movement restriction Complications Chronic paratenonitis can further progress into tendinopathy and tendon tears
- 117. Radiographic Features Ultrasound: On ultrasound, paratenonitis might appear as a linear hypoechoic lining around the tendon with associated hyperaemia on colour Doppler in chronic inflammation MRI: In the acute phase, a linear fluid-intense structure can be seen around the tendon. In the chronic phase soft tissue, scar-like structures can be seen extending into the peritendinous fatty tissue Differential diagnosis • tendinopathy • tendon tear • tendon rupture
- 118. Treatment and prognosis Treatment is usually conservative with nonsteroidal anti-inflammatory drugs, activity modification, physical therapy . Conservative Management Achilles tendon overuse injuries are initially managed with rest, ice, activity modification, and symptomatic analgesia. Eccentric Stretching: To counteract the failed healing response to repetitive subfailure loading, eccentric stretching has been proposed to facilitate collagen fiber cross-linking and promote tendon remodeling.
- 119. Physical Therapy As soon as possible after the initial injury, physical therapy should be started. The therapist should initially concentrate on isometric strengthening and eventually progress to range of motion exercises for the ankle and concentric triceps surae strengthening.
- 120. Tenosynovitis Tenosynovitis is inflammation of the lining of the sheath that surrounds a tendon (the cord that joins muscle to bone). Causes The synovium is a lining of the protective sheath that covers tendons. Tenosynovitis is inflammation of this sheath. The cause of the inflammation may be unknown, or it may result from: Diseases that cause inflammation, Infection, Injury, Overuse and Strain.
- 121. The wrists, hands, ankles, and feet are commonly affected because the tendons are long across those joints. But, the condition may occur with any tendon sheath. Symptoms Difficulty moving the joint Joint swelling in the affected area Pain and tenderness around the joint Pain when moving the joint Redness along the length of the tendon Treatment Using a splint or removable brace to help keep the tendons from moving to aid healing. Applying heat or cold to the affected area to help reduce pain and inflammation. Medicines such as nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injection to relieve pain and reduce inflammation. In rare cases, surgery to remove the inflammation around the tendon.
- 122. Physiotherapy Management Ice/Heat Packs - Heat can help relax and loosen tight musculature, and ice can be used to help relieve inflammation of the extensor sheath. Massage - Deep tissue massage at the thenar eminence can help relax tight musculature that causes pain. (See video). Graston Technique of manual soft tissue mobilization along with the eccentric exercise is also helpful. Graston technique includes breaking down fascia restriction, stretching connective tissue, and promoting a better healing environment. Stretching - Stretching the thenar eminence muscles into thumb extension and abduction can relax and lengthen this tight musculature that causes pain.
- 123. Strengthening exercise to increase strength Mobilization Therapeutic Ultrasound has also better outcomes in pain reduction and healing splinting Corticosteroid injections
- 124. Tendinosis Tendinosis is a chronic tendon injury. It is a common condition but is often misdiagnosed as tendinitis. Common in running athletes, young dancers, ice skaters and sports requiring frequent change of direction or jumping such as Characteristics Pain and, occasionally, swelling and warmth in the posterolateral aspect of the ankle along the course of the peroneal tendons.
- 125. Patients may relate exacerbation with rising onto the ball of the foot, running (lateral running, figure-8 running), cutting, jogging, or walking on uneven surfaces or following these activities or following a rest period, especially upon waking in the morning.
- 126. Outcome Measures LEFS (Lower Extremity Functional scale) FAAM (The Foot and Ankle Ability Measure) Medical Management The primary aim of treatment is to afford pain relief, restore mechanics and return the patient to their desired level of active participation Physiotherapy Management stretching, strengthening, mobilisation and manipulation, proprioceptive and balancing exercises, icing, ankle bracing or taping during contact sports If symptoms are severe, a cast or ROM boot immobilisation is prescribed for 10 days. After symptoms resolve, the patient begins a progressive rehabilitation programme along with a gradual increase to full activity.
- 127. The use of a biomechanical ankle platform (BAPS), deep tissue friction massage, ultrasound electric stimulation can also be included in the physical therapy
- 128. JOURNAL NAME Journal of Orthopaedic & Sports Physical Therapy TITLE AUTHOR Resistance Exercises in Early Functional Rehabilitation for Achilles Tendon Ruptures Are Poorly Described: A Literature Review (2020) Agres AN et.al METHODOLOGY To describe which resistance exercises are used in the first 8 weeks of treatment for acute Achilles tendon rupture and assess the completeness of reporting of the exercise descriptions. Randomized controlled trials, cohort studies, and case series (10 or more participants) that reported using resistance exercise in the immobilization period in the first 8 weeks of treatment for acute Achilles tendon rupture were included. OUTCOME MEASURES Short-term functional assessment of gait CONCLUSION A variety of resistance exercises targeted at the ankle plantar flexors were used as part of early functional rehabilitation after Achilles tendon rupture. However, most studies provided inadequate description of resistance exercise interventions.
- 129. JOURNAL NAME Orthopaedic Journal of Sports Medicine TITLE AUTHOR Does Early Functional Mobilization Affect Long-Term Outcomes After an Achilles Tendon Rupture? A Randomized Clinical Trial (2020) Susanna A et.al METHODOLOGY A total of 135 patients who underwent ATR repair, randomized to either EFM, including immediate postoperative loading and ankle motion, or standard treatment, were evaluated with functional tests and 5 self-administered outcome questionnaires at 6 and 12 months postoperatively. OUTCOME MEASURES Achilles tendon Total Rupture Score [ATRS] , Foot and Ankle Outcome Score [FAOS], The RAND-36 subscale of general health CONCLUSION This study demonstrated that an accelerated postoperative protocol with immediate loading and ankle motion resulted in better general health and vitality at 6 months. However, there were no differences between the groups in the recovery of heel-rise function.
- 130. INJURIES TO BURSA BURSITIS Bursitis is the inflammation of a bursa, a small fluid filled sac that sits between muscles, tendons and bones to reduce friction. Clinically Relevant Anatomy A Bursa appears at a junction of a tendon on the bone. A bursa is filled with a thin layer of synovial fluid. It protects and brakes the shocks of the joint. The structures nearby the bursa can move with minimal friction due to irritation. They have different measures and are mostly flattened.
- 131. Mechanism of Injury • Overuse of the joint: for example vacuuming for hours on end • Repetitive strain: for example picking up and lifting heavy loads • Trauma • Pressure • Bacterial infection: from an unattended wound (this is called septic bursitis) • Other inflammatory diseases: Gout for instance the gout crystals can form in the bursa and cause the inflammation. Etiology • Mainly by constant friction, thumping or pressure • The inflammation of the bursa frequently appears in combination with tendinitis • By an overuse injury or a trauma, especially when pulling and pushing heavy items • After a forced period of rest • There also can be an underlying rheumatic condition • Diabetes, osteoarthritis and disability of the thyroid gland can be associated with bursitis
- 132. Clinical Presentation There will likely be pain and discomfort over the affected area, and there will often be visible and/or palpable swelling. Diagnosis In most cases, bursitis can be diagnosed by physically examining the patient. Inspection • Redness and warmth can be signs of bursitis, but these symptoms are harder to spot when treating a Bursa that is not located superficially under the skin. • Local tenderness or stiffness. • Swelling can occur when inflammation gets worse. X-ray • Can rule out arthritis and bone deformities • Can sometimes confirm the presence of following substances inside the bursa (By which it become visible in X-ray) • Gout crystals • Calcifications: When the condition is chronic or recurrent. Bursa Fluid Punction: Can rule out infections.
- 133. Management Bursitis Due to Movement/Activity (Without Infection) • Rest the affected joint/ bursa • Ice packages • NSAID’s ( non steroid anti inflammatory drugs) • Injections with steroid agents • When improvement is noticeable, a gradual increase in exercise and activities is recommended. Note: Resting the affected joint does not mean immobilizing it, this could hold a risk towards adhesive capsulitis.
- 134. Bursitis Due to Infection ( Septic Bursitis) Antibiotics • Aspiration of the infected bursa fluid with the use of a sterile needle should be repeated approximately every 3 days • Never inject with steroids. • When the measures mentioned above are inadequate surgical interventions may be necessary in case of the following factors: • Surgical removal of the bursa is recommended in case of tuberculous bursitis • Surgical incision and drainage are recommended in case of : • Failure of adequately aspirating by needle • Bursa site inaccessible to multiple needle aspirations • Forming of abscess or necrosis
- 135. JOURNAL NAME International Journal of Physical Education, Sports and Health TITLE AUTHOR Effectiveness of shockwave therapy along with contrast bath and static Achilles stretch in patients with retrocalcaneal bursitis (2019) S Chahar et.al METHODOLOGY 30 patients having retrocalcaneal bursitis (female, male) fulfilling the inclusion and exclusion criteria were recruited and were randomly allocated in two groups. Group A subjects were given with contrast bath & Achilles stretch exercises and group B subjects were given ESWT along with contrast bath & Achilles stretch exercises. OUTCOME MEASURES Pain- VAS , AROM of ankle dorsiflexion (DF) & plantarflexion (PF), Roles and Maudsley’s (RM) score for functional ability. CONCLUSION Study proves that extracorporeal shockwave therapy has an additional effect in the management of retrocalcaneal bursitis.
- 136. JOURNAL NAME SVOA Orthopedics TITLE AUTHOR Effect of 4 Sessions of Low-Level LASER Therapy on Pain in Acute and Chronic Ankle and Foot Conditions (2022) S Kondal et.al METHODOLOGY Common acute and/or chronic ankle and foot conditions including Achilles tendinitis, Plantar fasciitis, Retrocalcaneal bursitis, Calcaneal spurs, pes planus/cavus, chronic ankle sprains were included in the study. Pain score was recorded OUTCOME MEASURES NPRS CONCLUSION LASER can be used in common ankle and foot conditions to reduce pain and improve tissue healing.
- 137. References • Clinical sports medicine : Peter Brunker and Karim Khan, third edition • Textbook of sports medicine : basic sciences and clinical aspects of sports injury and physical activity, Michael kjaer, Michael Krogsgaard • BRUKNER AND KHAN, CLINICAL SPORTS MEDICINE • Essential orthopedics: Maheshwari and Mhaskar 5th edition • Joshi and Kotwals essentials of orthopedics and applied physiotherapy, 4th edition • A meta-analysis by Doherty et al-Doherty, C., Delahunt, E., Caulfield, B., Hertel, J., Ryan, J., & Bleakley, C. (2014). The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis • Recurrence rates amongst basketball players is reported to be greater than 70%-Yeung, M. S., Chan, K. M., So, C. H., & Yuan, W. Y. (1994). An epidemiological survey on ankle sprain. British journal of sports medicine, 28(2), 112-116.
- 138. • Clinically relevent anatomy-Malleolar fractures: nonoperative versus operative treatment. A controlled study. Bauer M, Bergström B, Hemborg A, Sandegård J. Clin Orthop Relat Res. 1985 Oct; (199):17-27. • A previous sprain may compromise the strength and integrity of the stabilisers and interrupt sensory nerve fibres- Beynnon, B. D., Murphy, D. F., & Alosa, D. M. (2002). Predictive factors for lateral ankle sprains: a literature review. Journal of athletic training, 37(4), 376 • Mechanism of injury-Hubbard, T. J., & Hicks-Little, C. A. (2008). Ankle ligament healing after an acute ankle sprain: an evidence-based approach. Journal of athletic training, 43(5), 523. • Reports has proposed that-Wright, I. C., Neptune, R. R., van den Bogert, A. J., & Nigg, B. M. (2000). The influence of foot positioning on ankle sprains. Journal of biomechanics, 33(5), 513-519 • Van der Wees PJ, Lenssen AF, Feijts YAEJ, Bloo H, van Moorsel SR, Ouderland R, et al. KNGF-Guideline for Physical Therapy in patients with acute ankle sprain. Dutch J Phys Ther. 2006
Editor's Notes
- Treatment comprises early reduction of the dislocation, and frequently involves open reduction internal fixation to restore and stabilise the talonavicular joint. Open reduction and fusion of the calcaneocuboid joint is occasionally required

TUTORLISTENING.COM
(from IELTS TUTOR )
- IELTS TUTOR Hall of fame
- Chính sách IELTS TUTOR
- Câu hỏi thường gặp
- Thời gian thi
- All Categories
- Tourism and Travelling
- Pronunciation
- Health and Medicine
- Social issues
- IELTS Advice
- Đề thi thật IELTS
- Environment
Presentation on foot injuries among sports players: Đề thi thật IELTS LISTENING Vol 1 Test 2 Section 3
Bên cạnh PHÂN TÍCH ĐỀ THI THẬT TASK 2 (dạng advantages & disadvantages) Some students work while studying. Discuss the advantages and disadvantages of this trend and give your opinion?NGÀY 04/8/2020 IELTS WRITING GENERAL MÁY TÍNH (kèm bài được sửa hs đi thi) , IELTS TUTOR cung cấp Presentation on foot injuries among sports players: Đề thi thật IELTS LISTENING Vol 1 Test 2 Section 3
I. Kiến thức liên quan
IELTS TUTOR lưu ý:
- Cách học IELTS LISTENING hiệu quả
- Khắc phục mất tập trung khi nghe IELTS LISTENING
- Tự học IELTS LISTENING từ A-Z
II. Presentation on foot injuries among sports players: Đề thi thật IELTS LISTENING Vol 1 Test 2 Section 3
Questions 21-26
Choose the correct letter, A, B or C.
Presentation on foot injuries among sports players
21 John and Cath's presentation plans are different in
A the examples used.
B the order of information .
C the main points made.
22 What do the students agree about the anatomy section of their presentation?
A It would be better if Gath spoke about it.
B It should be kept quite short.
C It should be based on information from the internet. >> IELTS TUTOR lưu ý: PHÂN TÍCH ĐỀ THI TASK 1 VIẾT THƯ NGÀY 05/7/2020"you are going to take a holiday and your friend agrees to stay at your house. Write a letter to him for"IELTS WRITING GENERAL MÁY TÍNH (kèm bài được sửa HS đạt 6.0 đi thi thật)
23 What do the students agree to include in the last section?
A visuals of injuries
B demonstrations of treatment
C interviews with patients
24 What is said about the different types of heel injury?
A Diagnosis is straightforward.
B They are expensive to treat.
C Some are more serious than others.
25 On the subject of causes of heel injuries, the students agree to
A focus on a single reason.
B reject certain approaches.
C use a source written by their professor.
26 What does Gath say about stretching as a treatment?
A It is potentially risky.
B It is commonly confused with strengthening,
C It is the least effective part of treatment. >> IELTS TUTOR lưu ý: PHÂN TÍCH ĐỀ THI THẬT TASK 2 (dạng advantages & disadvantages) Some students work while studying. Discuss the advantages and disadvantages of this trend and give your opinion?NGÀY 04/8/2020 IELTS WRITING GENERAL MÁY TÍNH (kèm bài được sửa hs đi thi)
Questions 27 and 28 Choose TWO letters A-E.
Which TWO treatment techniques did the female runner find useful for her swollen heel?
B ultrasound
D balancing exercises
Questions 29 and 30 Choose TWO letters, A-E.
Which TWO sports did the male sprinter find most effective during his rehabilitation programme?
B weight-training
C running on grass
E jumping >> IELTS TUTOR lưu ý: Phân tích"Some people do not mind to spend their leisure time with their colleagues while some people prefer to keep their private life separate from their work life. Is it a great idea to spend leisure time with your colleagues?"IELTS WRITING (kèm bài viết thi thật HS đạt 6.0)
III. Đáp án Presentation on foot injuries among sports players: Đề thi thật IELTS LISTENING Vol 1 Test 2 Section 3


IMAGES
COMMENTS
Sep 18, 2022 · Presentation on foot injuries among sports players. 21. John and Cath’s presentation plans are different in. A. the examples used. B. the order of information. C. the main points made. 22. What do the students agree about the anatomy section of their presentation?
John and Kath are preparing a joint presentation on foot injuries in sports players. They have similar presentation structures focusing on anatomy, injuries, and treatment. They discuss dividing the topics: John will cover anatomy and types of heel injuries while Kath will discuss stretching techniques. They plan to include case studies at the end to illustrate treatment. One case discusses a ...
John and Kath are preparing a joint presentation on foot injuries in sports players. They discuss structuring their presentation to include sections on anatomy, injuries, and treatment. John will cover anatomy while Kath suggests demonstrating treatment techniques by acting as a patient. They agree different types of heel injuries vary in severity and discuss causes like overuse or sudden ...
The percentages of foot injuries per sport for female and male athletes are presented in Figure 1A. Values ranged from 15.1% for men's cross-country running to 2.5% for men's wrestling. The foot-injury rates by sport and sex, expressed in foot injuries per 10 000 AEs, are shown in Figure 1B. The highest injury rate was in women's gymnastics (10 ...
Data was extracted from the included studies by three authors (SS, PK and RR); the following parameters were recorded: (a) country and year of publication (b) total number of athletes included (c) total number of injuries reported (d) total foot and ankle injuries reported (e) age and sex distribution (f) sport-wise distribution (g) specific ...
May 2, 2023 · Sports-related foot and ankle injuries are a common occurrence among athletes of all levels, and can range from minor sprains to severe fractures. The feet and ankles are complex structures that are composed of bones, joints, ligaments, tendons, and muscles, which are all susceptible to injury. The most common types of sports-related foot and ankle injuries include sprains, strains, fractures ...
Apr 8, 2022 · 7. Pott's fracture • It is one of a common sporting inversion injury especially in jumping sports (e.g. basketball, volleyball). • They are usually a result of a forced plantarflexion/inversion movement, whereby the complex of ligaments on the lateral side of the ankle is torn by varying degrees • Inversion injuries are also far more common than eversion injuries due to the relative ...
Đáp án Presentation on foot injuries among sports players: Đề thi thật IELTS LISTENING Vol 1 Test 2 Section 3 Các khóa học IELTS online 1 kèm 1 - 100% cam kết đạt target 6.0 - 7.0 - 8.0 - Đảm bảo đầu ra - Thi không đạt, học lại FREE
May 1, 2014 · The most common site of injury in soccer player is the lower extremity. Breaking it down further, the most injured joint is the ankle joint (0.17–6.52 per 1000 person hours), followed by the knee and the thigh [1]. Of all foot and ankle injuries, ankle sprains are the most common (80%), then bruises (9-49%), and tendon lesions (2-23%) (Table 1).
Apr 1, 2022 · Other injuries which is also common in football players are such as, ligament of knee, hamstring strain, football concussion, wrist injury. Discover the world's research 25+ million members